Identifying and locating superior gluteal artery perforator on Vietnamese adults – A study for clinical applications
Abstract
The superior gluteal artery (SGA) perforator flap (SGAP) used to cover lumbosacral soft tissue defects, in order to take advantage of the SGAP flap, all surgeons are required to have substantial knowledge of its cutaneous distribution of perforator. This study describes the anatomical characteristics of the perforators of SGA on Vietnamese adults; and locates the perforator of SGA on the gluteal region. We carried out on 32 Vietnamese adult cadavers at Department of Anatomy of Ho Chi Minh University of Medicine and Pharmacy, from Jan 2017 to June 2019. On average, SGA gives off 4-5 perforators, while none was found on the deep branch. The average length of perforator from the skin to the dissecting point is short compared to that of from skin to origin diameter at origin is quite large (1mm). The chance of finding 3-5 perforators in the upper triangle is 75% and 87% on the right and left side, respectively. Also, the probability of finding a single perforator in the upper triangle is 100% based on the x-axis, most perforators are found in segment 2/5 to segment 3/5 with the center being the midpoint between two segments; based on the y-axis, most perforators are found in segment 1.5/5 to segment 3.5/5 with the center being the midpoint between the two.
INTRODUCTION
Nowadays, there are many prevention modalities used to counteract the debilitating outcomes of pressure ulcers as well as definitive treatments to reconstruct the lumbosacral soft tissue defect using septocutaneous flap, gluteus maximus myocutaneous flap or free flap [1] [2, 3]. When a free flap is used, the microsurgical reconstructive material must meet specific anatomic, functional and cosmetic requirements of the donor site as well as those of recipient site, in which tissue amount and quality, consistency and compatibility of flap pedicle, etc. Pedicled flap and free flap are two ways that a SGAP flap can be used to reconstruct soft tissue defects. In 1993, Koshima et al was the first to use SGAP flap as an advancement flap or a rotation flap to cover lumbosacral defects in 8 patients whose great outcomes could be attributed to its great rotational arc and adequate flap thickness [4, 5]. Surgeons need to have a profound understanding of the anatomy of the pedicle supplying the flap, especially its course and cutaneous visualization of the SGAP. The perforators can be found in two ways: (1) a line is drawn from the posterior superior iliac spine (PSIS) to the coccyx (C), and another from the PSIS to the apex of the greater trochanter. At the midpoint of the line connecting the PSIS and coccyx, draw another line from the cranial edge of the greater trochanter then mark a point in the medial third of the line connecting the PSIS and greater trochanter as this is where the SGA exits the pelvis via the suprapiriform foramen. SGAPs are mostly found in the middle third region of the line connecting the PSIS and greater trochanter; and (2) using Doppler ultrasonography to mark the cutaneous insertion of the perforator based on the spectrum in the aforementioned triangular region, which is used to locate the perforator [5] [2, 3]. However, in Vietnam, no author has ever investigated the cutaneous insertion pattern of the SGAP in Vietnamese adults while foreign counterparts had long studied its anatomy [6]. Therefore, identifying the origin, course, perforator type and locating the cutaneous insertion of perforator have crucial impacts on flap elevation surgery used to cover soft tissue defects or microsurgical free flap reconstruction [1-3].
With these necessities in mind, we initiated this research to investigate the anatomical characteristics of SGAP and to find the cutaneous insertion pattern of SGAP in the buttocks of Vietnamese adults. There were two main objectives in this study: (1) Describe the anatomical characteristics of the perforators of SGA on Vietnamese adults, and (2) Locate the perforator of SGA on the gluteal region.
MATERIALS AND METHODS
Materials
Dissections were performed on the gluteal region of 32 formalin-preserved Vietnamese adult cadavers, including both male and female, at the Department of Anatomy of Ho Chi Minh University of Medicine and Pharmacy from Jan 2017 to Jun 2019. Therefore:
We obtained a convenience sample of readily available cadavers with the following inclusion criterion:
(1) Vietnamese adult cadaver, 18 years old and above.
(2) Intact gluteal region with no past surgical history
(3) No visible deformities, tumors or anatomical abnormalities in the gluteal region
Exclusion criterion: exclude specimens whose gluteal region are deformed or previously operated on.
Equipment
Standard classical dissection kit, vernier caliper, compass, 4x magnifying loupe. Sony Alpha 7 mark II full-frame mirrorless camera with Sony Zeiss FE 24-70mm f/4 lens equipped.
Protocols
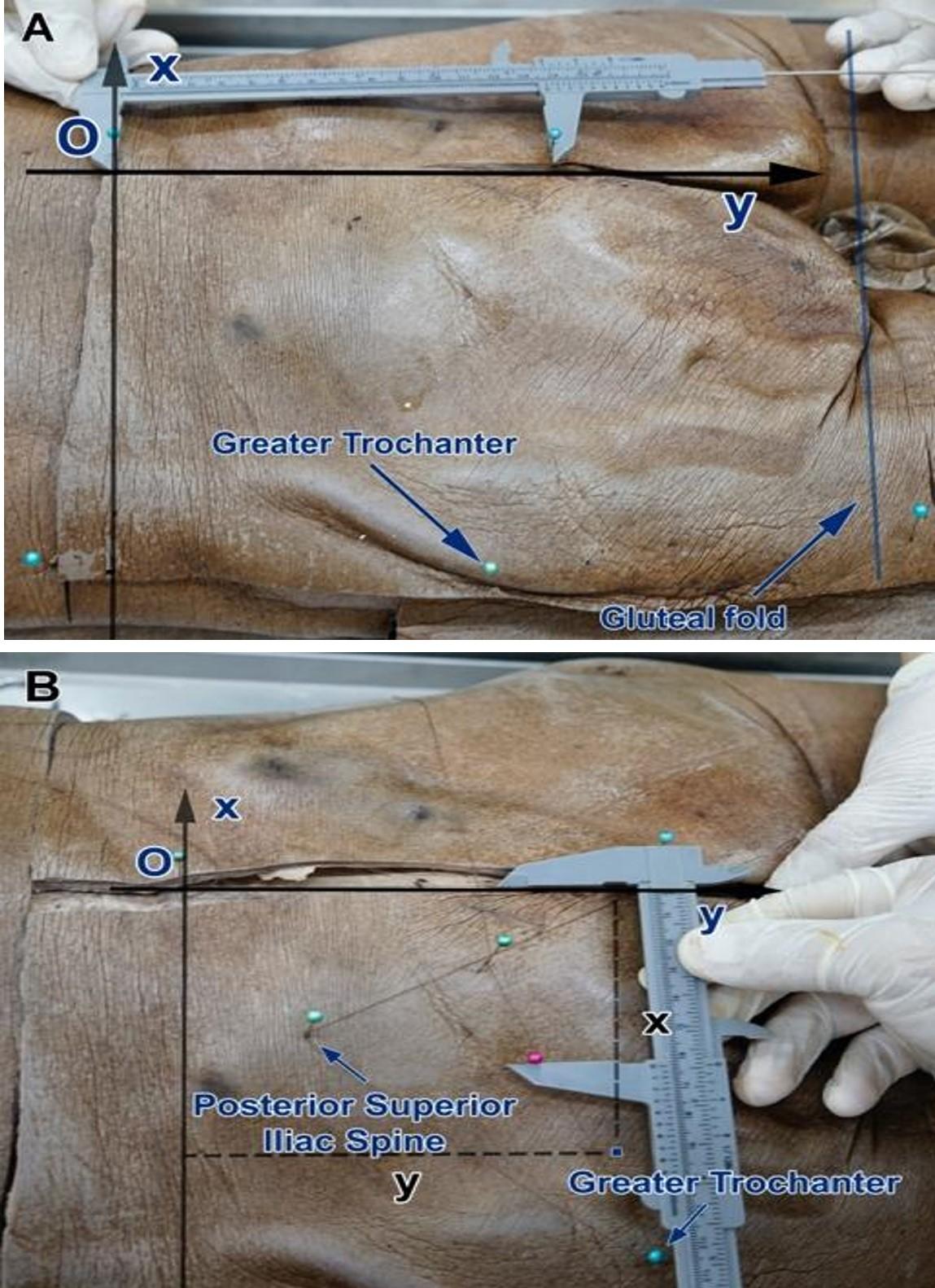
Gluteal dissection was performed as following: made an incision along the line connecting the two anterior superior iliac spine (ASIS, x-axis), then made another incision along the intergluteal cleft (y-axis) so that it’s perpendicular to the x-axis and meet the x-axis at a point called the origin (point O); made another incision along the gluteal sulcus then make another one from the ASIS to the gluteal sulcus so that it’s parallel to the y-axis. The origin (O) is the point where the intergluteal cleft (y-axis) intersects the dorsally projected interconnecting ASIS line (x-axis). Next, we took these measurements: the distance between the uppermost point of the intergluteal cleft and point O, the distance between point O and ASIS, intergluteal cleft length, and the distance between interconnecting ASIS line and left and right gluteal sulcus (Figure 1A-B)
The dissection continued along the vessels’ interseptal course to enter the plane underneath the gluteus maximus and medius muscles in order to trace back to the origin of the SGA. After having dissected the gluteus maximus and medius muscles, we reached the gluteal deep layer and then identified the piriformis muscle as well as the superior and inferior gluteal neurovascular bundles. Next, dissected the origin of SGA and its superficial and deep branches. From the superficial branches, we continued following the musculocutaneous and septocutaneous perforators. On the other hand, we did not document any perforators branching off the SGA’s deep branch, and only branches supplying the muscles were recorded.
We documented the number of superficial branches, branches that supply the muscles, musculocutaneous and septocutaneous branches. In addition, the origin of each perforator, the length from the overlying skin to the dissecting point, the length from the overlying skin to the SGA origin, the cutaneous diameter as well as its diameter at origin were all identified; musculocutaneous and septocutaneous types were recorded; the perpendicular or oblique course was also noted. Additionally, we obtained the location and coordinates of each perforator, together with the following parameters: the distance between the greater trochanter and PSIS, the distance between the greater trochanter and coccyx, the distance between PSIS and coccyx, the distance between the greater trochanter and the midpoint of the line connecting PSIS and coccyx. Based on this triangle, we determined the coordinates and location of each perforator (x, y), and whether the perforator lies in the upper or lower triangle.
While dissecting the skin from the subcutaneous fat, we noticed that the gluteal subcutaneous fat is quite thick. Continued dissecting the gluteal subcutaneous fat carefully and watch out for exit points of perforators. Then, dissected along the lateral border of the gluteus maximus muscle while paying attention to the septocutaneous perforators of the superficial branch of the SGA that could run through the interseptal plane between the gluteus maximus and medius muscles.
Data collection
Origin of perforators, musculocutaneous or septocutaneous types were all collected. In addition, we determined whether the perforator’s course was perpendicular or oblique. Furthermore, the distance between the uppermost point of the intergluteal cleft to point O, the distance between point O and ASIS, the length of intergluteal cleft, the distance between the ASIS line to the bilateral gluteal sulci were obtained. Additionally, we took the measurements of the distance between the greater trochanter and the PSIS, the distance between the greater trochanter and coccyx, the distance between PSIS and coccyx, the distance between the greater trochanter and midpoint of the line connecting PSIS and coccyx. All of the above measurements were used to locate the perforators by means of the Cartesian coordinate system. In addition, we also documented whether the perforator lies in the upper or lower triangle.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study was approved by certificate number 166B/BVCR-HĐĐĐ 10/9/2015. The source of cadavers belongs to the Department of Anatomy of Ho Chi Minh University of Medicine and Pharmacy.
Statistical analysis
Qualitative variables were described, and quantitative variables were measured. Percentages and mean values of variables were analysed using chi-squared test when comparing the percentage of each variable and paired t-test when comparing average values between each side. Statistical analyses were performed using SPSS/PC 21.0.
RESULTS
Origin, number, type, course and dimensions of perforators
The superficial branch of the SGA gives off 3 to 6 perforators, and the ratio of 5 to 6 perforators is quite high, about 62.5% on the right and 43.8% on the left (Table 1). The percentage of muscular perforators from the right superficial branch and left superficial branch accounts for 70% and septal perforator 30% on both sides (Figure 2A-B).
On average, the superficial branch of the SGA gives off 4.6±1.1 and 4.4±0.9 perforators on the right and left side respectively (no significant difference between right- and left-sided distribution of perforators was found (p=0.32). Besides, we were not able to identify any perforators coming off the deep branch. The chance of perforators coming off the superficial branch is described below (Table 1). The superficial branch gives rise to 3-6 perforators and none was identified coming off the deep branch.
Our observations revealed that 100% of the perforators arising from the superficial branch will reach the skin in an oblique orientation. We found that the length of the perforator from skin to the dissection point is short (5.5-7.5mm) compared to that of from skin to SGA’s origin (4-9cm). We also observed that the diameter at the origin of the perforator is quite large (over 1mm) compared to that of at the terminal end at the cutis (less than 0.5mm). The dimensions between left-sided and right-sided perforators aren’t found to be statistically significant for p ≥ 0.05. We classified the diameter at the origin of the perforator arising from the superficial branch over 1mm which accounts for 50% and from 0.5-1mm which accounts for 95% on both sides; no significant difference between the diameter at origin of perforator on both sides (p≥0.05 ) (Table 2)
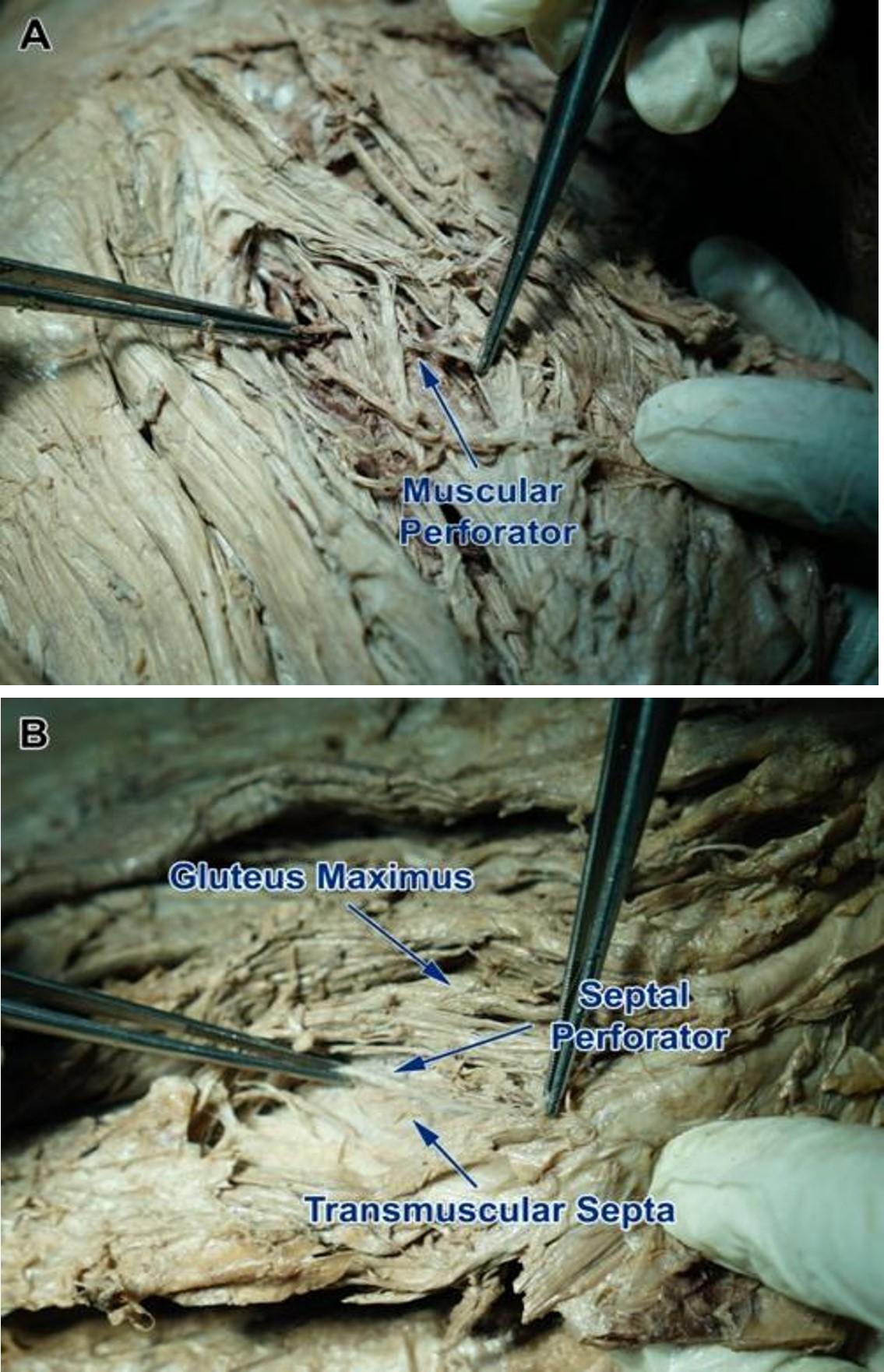
Table 1. Chance of perforators coming off the superficial branch.
Table 2. Classification of diameter at origin of perforators rising from superficial branches.
Cutaneous projection of the perforators on the buttocks
On average, the distance from the greater trochanter to the PSIS is 15cm, while the distance from the greater trochanter to the midpoint of a line connecting the PSIS and coccyx is 13.5cm. We also found that the distance from the midpoint of the line between the PSIS and coccyx to the PSIS is approximately 6.5cm (Table 3). The triangles’ dimensions between the left and right side is not shown to be statistically significant (p ≥0.05).
Additionally, the chance of finding 3-5 perforators found in the upper triangle is 75% and 87% on the right and left side respectively. Furthermore, the probability of finding a single perforator in the upper triangle is 100% (Figure 3A). No significant difference was identified between the left and right-sided probability of finding perforators in the upper triangle (p ≥0.05) (Table 4). However, we only identified perforators in the lower triangle in 5/16 specimens and most specimens were shown to only have a single perforator which comes from the SGA’s superficial branch. The majority of the perforators are located in the upper triangle on both the right and left side, while the chance of finding perforators rising from the SGA’s superficial branch is negligible.
There were no significant differences between the left and right-sided coordinates of perforators (p≥0.05). Based on the coordinates, we are able to calculate the ratio of coordinates of the SGAP and map the frequencies of perforator segment in the gluteal region.
On the basis of ratio of coordinates in Table 6 above, we were able to determine the location of perforators by dividing x- and y- axes into 5 equal line segments, each of which is 3.5cm long (Figure 3B):
(1) X-axis (from point O to bilateral ASIS): we divided the x-axis into 5 equal segments (with segment no. 1 lies nearest to point O, and segment no. 5 lies farthest from point O), the regions where most perforators are mostly found are from segment no. 2/5 to segment no. 3/5 with the center being the midpoint between both segments.
(2) Y-axis (from point O to the endpoint of the intergluteal cleft): we also divided the y-axis into 5 equal segments (with segment no 1 lies nearest to point O, and segment no. 5 lies farthest from point O), the regions where most perforators are mostly found are from segment 1.5/5 to segment 3.5/5 with the center being the midpoint between both segments.
(3) The region that perforators are mostly concentrated is a rectangle that has a length of 7 cm (2 segments) and a width of 3.5 cm (1 segment); its center is the intersection of two lines, each of which bisects the x-axis and y-axis; and this rectangle lies within the upper triangle which occupies more area than that of the lower one.
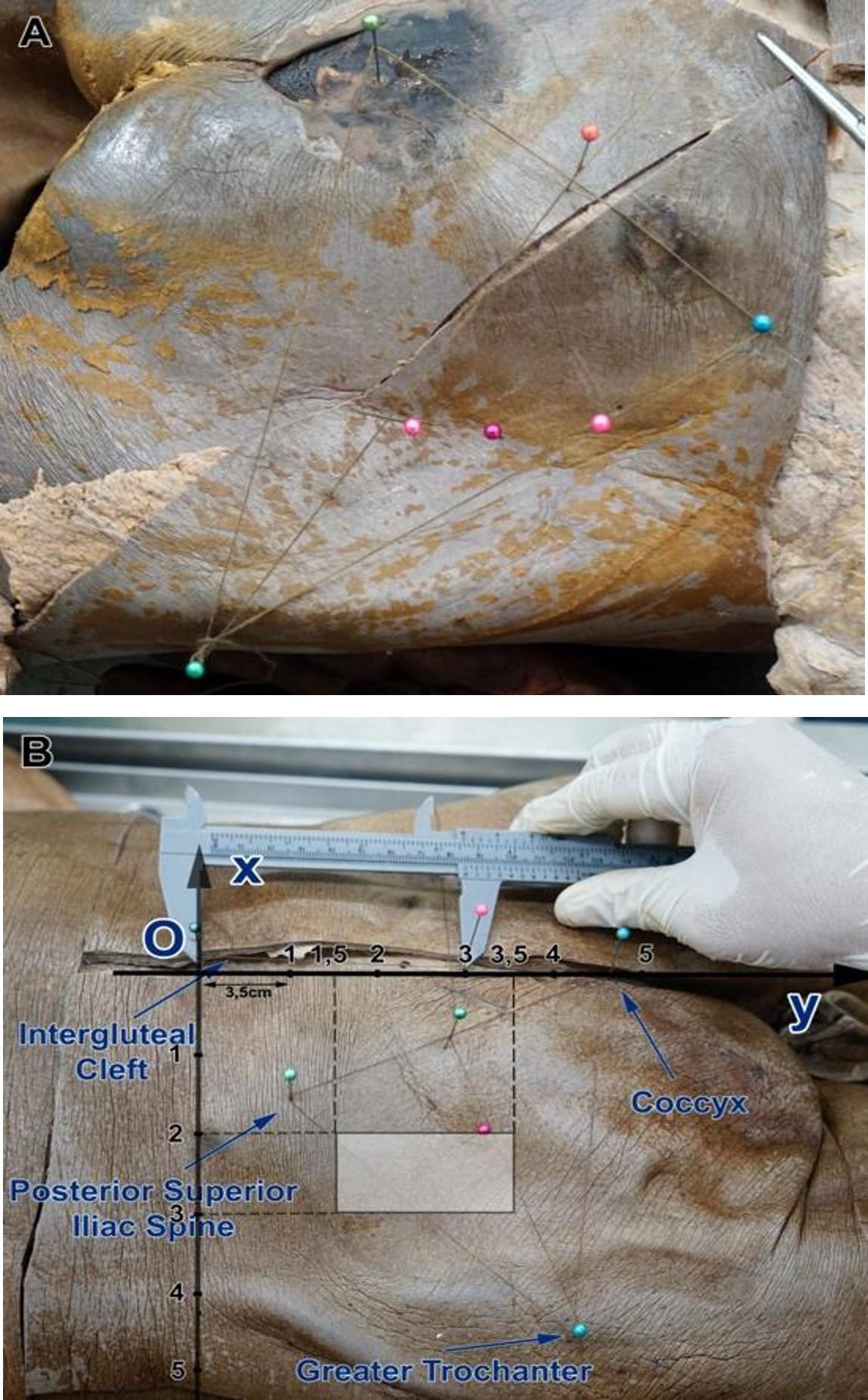
Table 3. Dimensions of gluteal triangles used to locate perforators.
Table 4. Number of perforators in superficial triangle.
Table 5. Coordinates of perforators.
Table 6. Ratio of coordinates of SGAP.
DISCUSSION
During the dissection, we documented that approximately 4 to 5 perforators were arising from superficial branch of SGA with the chance of finding 5-6 perforators being 62.5% and 43.8% on the right and left side respectively, which was quite high. No perforators can be found arising from the deep branch, this can be explained by (1) the fact that the dissection becomes increasingly difficult to maintain the vessel integrity due to the perforator’s small size and deep course, and (2) the fact that the deep branch that runs between the gluteus medius and minimus muscles only supplies the muscles around it and therefore does not give rise to any perforator. This concurs well with a study of Park et al [2] in Korean adults which stated that 4-5 perforators originate from the SGA. Cadaveric dissection studies showed that the number and location of perforators arising from SGA vary greatly, with an average amount of 3-5 large perforators arising from the SGA (amount of perforators can fluctuate from 1-7 vessels) [1]. Our findings, which corroborate with previous results by Ahmadzadeh et al [1], show that the upper gluteal region is supplied by 5±2 perforators which stem from the SGA. However, a domestic study of Vu Quang Vinh and Tran Van Anh (2011) [6] showed that the amount of perforators supplying the SGAP flap to repair lumbosacral defects is usually 2-3 perforators.
The percentages of muscular perforators from the superficial branch between both sides are similar, in which the muscular and septal type account for 70% and 30% respectively. We also found that 100% of perforators will reach the skin in an oblique orientation. In addition, our findings revealed that both musculocutaneous and septocutaneous will certainly have an intramuscular or intermuscular septal course before terminating at the skin. As a result of its long oblique course, the pedicle length will be also longer. However, when using the SGAP flap to cover lumbosacral defects, since the flap design usually lies next to the defect, dissection of perforator flap pedicle to rotate the flap to cover the defect does not necessitate long perforator flap pedicle and therefore stopping the dissection at the gluteus maximus is enough to cover the defect. This finding is consistent with the date reviewed by Hashimoto I. et al [7] which revealed that the SGA gives rise to a vertical arrangement of perforators that go straight into the superficial tissue above the muscles. The vertical arrangement of perforators is preferred due to its resultant post-dissection pedicle length. Hashimoto also showed that, according to his expertise, he could pedicle the SGAP flap on a single perforator without having any risk of flap necrosis. Our results are similar to Granzow J.W et al.’s [8] findings in which they found perforators supplying the medial portion of the buttocks have short intramuscular lengths while perforators supplying the lateral portion of the buttocks will have an oblique course through the muscle. Therefore, pedicles based on perforators from the lateral aspects of the skin paddle tend to be longer than those based on more medial perforators. In contrary to earlier findings by Hashimoto and Granzow, Vasilee J.V. et al.’s studies [7-9] showed that perforators course through the gluteus maximus and medius muscles at a variety of angles and distances. The perforators usually go through the gluteus maximus muscle at a more acute angle which can result in a shorter skin incision as well as create a SGAP flap having a shorter pedicle length (6-8cm).
We also agree with Tuinder S.’s findings [4], which stated that the perforator course is a secondary factor influencing the choice of perforator. If both vessels have the same dimensions and subcutaneous branching characteristics, whichever perforator is easier to dissect or less traumatizing to muscles will be chosen. Instead of the pedicle which has a sufficient length to cover the defect, single perforator-based flap with a direct course into muscles will be chosen because it operates easier and faster with less damaging effects to gluteus maximus muscle, although hypothetically septal perforators are more advantageous thanks to its muscle-sparing effect on the gluteus maximus muscle when flap harvesting [1]. According to our study, when it comes to choosing or disregarding a perforator when dissecting, we can always rely on Doppler ultrasonography to choose whichever one that has a larger spectrum.
According to Sung K.W.’s study [10], ascending and transverse branches of the superficial branch of the superior gluteal artery are difficult to dissect because they don’t follow along the muscle fibers’ direction. The main descending branch has a longer pedicle and a parallel course to muscle fiber, which is completely consistent with our findings. However, dissecting this branch is an extremely demanding and dangerous task due to the gluteus maximus thickness at the insertion point of the perforator as well as that of tensor fasciae latae.
Average perforator internal diameter is 1-1.5mm, in which vessels that have 1mm diameter account for 50% and those that have 0.5-1mm diameter account for 95% on both sides. The length of perforator from skin to the dissection point is quite short (5-8mm) compared to that of from the skin to its origin (4-9cm). This finding is mostly consistent with a previous study by Lin et al [11], which showed that perforators have 1-1.5mm diameter and 3-8cm in length. Ahmadzadeh et al.’s [1] observations showed that perforator have diameter of 0.6-1.0mm and average pedicle length from deep fascia of 2.3±1.1mm. Another study by Tansatit showed that perforators have an external diameter of 0.5 to 1.7mm (mean value is 1.2mm) and pedicle length from skin to main artery of 3-11.5cm (mean value is 5.9 cm) [5].
According to Vasile J.V et al [9], the most mandatory factor for an optimum perforator at the base of the pedicle is the size of the perforator, its pedicle length, the position where the pedicle enters the flap, and the subcutaneous branching patterns of vessels. The larger the vessel is, the more sufficient the pedicle will be for flap transplant; the center position of the vessel on the pedicle and the branching characteristics for graft perfusion are preferred. Based on their findings, we believe that SGAP diameter and length are strong points when using this kind of flap and this is also consistent with others’ findings.
The chance of finding 3-5 perforators in the upper triangle is 75% on the right side and 87% on the left side; a single perforator can be found 100% of the time in the upper triangle. However, perforators in the lower triangle are only present in 5/16 cadavers; most of the time only a single perforator is found and also belongs to the superficial branch of the SGA. In general, the majority of perforators are mostly located within the upper triangle on both sides while the chance of finding a perforator in the lower triangle is small, and therefore, negligible. The prime cause for this result is the fact that we divide the large triangle into 2 smaller and equal ones by a line connecting the greater trochanter to the midpoint between PSIS and coccyx. Therefore, when we look at the distribution, the perforators tend to aggregate in the upper triangle and sometimes 1-2 perforators are found asymptotically with the lower side of the upper triangle. This finding isn’t clinically relevant, but can act as a warning to surgeons when they use ultrasonography preoperatively to look for perforators in the upper triangle and they should also focus on the asymptotic lower side.
This result is also consistent with the localization method of Hallock G.G [12] in which they locate the SGAP by drawing a line from the PSIS to coccyx and another from the PSIS to the greater trochanter. At the midpoint of the line between PSIS and coccyx, another line is drawn from the cranial edge of the greater trochaner that will be equivalent to the course of the piriformis muscle. After that, mark a point at the medial third of a line between PSIS and the greater trochanter. This point is where the SGA exits the pelvis through the suprapiriform foramen. The main perforator of the SGA is found at the transverse and distal portion of this exit point and is also found superior to the piriformis muscle. In recent studies, Ahmadzadeh et al.’s study showed that they mostly found the SGA in the two third of a line between the PSIS and the greater trochanter. Also, another study by Tansatit T. (2008) [5] revealed that the perforators are arranged in a line along the upper and lateral free border of the gluteus maximus muscle and this line is parallel inferiorly by a line marked by connecting the PSIS and greater trochanter. However, in our study, we only find a linear distribution of perforators in 1 specimen.
Nevertheless, during our dissection and flap harvest, we realize that locating 2 landmarks which are the greater trochanter of the femur and the PSIS can be relatively difficult in obese patients whose buttocks can contain a lot of fat. Our findings are consistent with that of Kim et al [13] in which they documented superior gluteal flap adjacent in the superomedial region has the least thickness while the thickest is the superolateral region, whose area can be 3.24 times larger than that of the former. The flap tended to be thicker in the direction of the thinnest superomedial area to the inferomedial area than in the superior area. Therefore we chose our point of origin to be the midpoint of the dorsally projected interconnecting ASIS line (ASIS is an easy-to-identify landmark on both thin and obese patients) (x-axis) and from point O a line is drawn along the intergluteal cleft to the coccyx (y-axis). Then, we tried to locate the perforators’ coordinates by mapping this coordinate system on the gluteal region. Our results showed that the region at which most perforators can be found along the segment 2/5 to segment 3/5 with the center being the midpoint of the two segments (about 3.5cm) on the x-axis and segment 1.5/5 to segment 3.5/5 with the center being the midpoint of the two segments (about 7cm). Based on this result, the majority of perforators can be found within a rectangle with a length of 7cm (two segments) and a width of 3.5cm (1 segment) with its center being the intersection between two perpendicular bisectors of the x- and y- axis on both sides respectively. This rectangle lies within the upper triangle whose area occupied more area than the lower one. Our findings revealed that a perforator distribution pattern is easily applicable in the clinical context because it lies within a rectangle (which can be divided into 5 equal segments) and it also supplements and substantiates previous concepts by other authors. A previous study by Hallock G.G [12] showed that in order to identify SGAP, draw a line connecting the PSIS and the coccyx, and a line from PSIS to the apex of the greater trochanter. Then connect the midpoint of the line connecting the PSIS and coccyx to the point at the cranial edge of the greater trochanter. This line is equivalent to the course of the piriformis muscle. Next, mark a point at the medial third of the line connecting the PSIS to the greater trochanter. This point is where the SGAP exits the pelvis through the suprapiriform foramen. The main perforator of the SGA is found at the transverse and distal portion of this exit point and cranially to the piriformis muscle. In recent studies, Ahmadzadeh et al hypothesized that they mostly found the SGA in the middle third of the line connecting the PSIS to the great trochanter. A study by Gagnon A.R. et al. [3] used a similar coordinate system similar to that of our method, in which they draw a rectangle based on the PSIS-greater trochanter axis in order to locate the perforators, while our method uses a vertical coordinate system. As a result, our method has a better chance of finding the SGAP.
CONCLUSION
The superficial branch of the SGA usually gives off 5 cutaneous perforators in which 5-6 perforators account for 62.5% and 43.8% on the right and left side respectively. No perforators were found branching off the deep branch of the SGA. The perforator length from skin to the dissection point is short compared to the length from skin to its origin. Vessels with diameter at origin from 0.5-1mm account for 95% on both sides.
Chance of finding 3-5 perforators in the upper triangle accounts for 75% and 87% on the right and left side respectively and the probability of finding a single perforator in the upper triangle is 100%. Using a two-dimensional system (x-axis, y-axis). We’re able to visualize a rectangle containing the SGAP perforators with a length of 7cm (2 segments) and a width of 3.5cm (1 segment) with its center being the intersection of two bisectors of the x- and y-axis; this rectangle is found within the upper triangle whose area occupied more area than the lower one.
FUNDING
No funding was received for this study
ACKNOWLEDGEMENT
We would like to thank Nghia Pham (10900 Euclid Ave., Cleveland, OH, 44106, Department of Biomedical Engineering, Case Western Reserve University) for critical reading and checking to improve the manuscript.
CONFLICTS OF INTEREST
Authors declared that they have no conflict of interest.
References
- [1]Ahmadzadeh R, Bergeron L, Tang M, Morris SF. The Superior and Inferior Gluteal Artery Perforator Flaps. Plastic and Reconstructive Surgery. 2007;120:1551-1556.
- [2]Park HJ, Son KM, Choi WY, Cheon JS. Clinical Efficacy of Gluteal Artery Perforator Flaps for Various Lumbosacral Defects. JKSM. 2016;25:49-55.
- [3]Gagnon AR, Blondeel PN. Superior Gluteal Artery Perforator Flap. Semin Plast Surg. 2006;20:79-88.
- [4]Stefania Tuinder, Rene Van Der Hulst, Marc Lobbes, Lataster BVaA. Septocutaneous Gluteal Artery Perforator (Sc-GAP) Flap for Breast Reconstruction: How We Do It. Breast Reconstruction – Current Perspectives and State of the Art Techniques: IntechOpen; 2013. p. 135-160.
- [5]Tansatit T, Chokrungyaranont P, Sanguansit P, Wanidchaphloi S. Anatomical study of the superior gluteal artery perforator (S-GAP) for free flap harvesting. Journal of the Medical Association of Thailand = Chotmaihet thangphaet. 2008;91:1244-1249.
- [6]Vinh V.Q, T.V. A. Applied research of supeior gluteal artery perforator flap in treantment for sacral pressure ulcers (Nghiên cứu ứng dụng vạt da nhánh xuyên động mạch mông trên trong điều trị loét vùng cùng cụt do tì đè). Journal of Disaster Medicine and Burn injuries 2011;2:208-214.
- [7]Hashimoto I, Abe Y, Ishida S, Kashiwagi K, Mineda K, Yamashita Y, et al. Development of Skin Flaps for Reconstructive Surgery: Random Pattern Flap to Perforator Flap. The Journal of Medical Investigation. 2016;63:159-162.
- [8]Granzow JW, Levine JL, Chiu ES, Allen RJ. Breast reconstruction with gluteal artery perforator flaps. Journal of Plastic, Reconstructive & Aesthetic Surgery. 2006;59:614-621.
- [9]Vasile JV, Newman T, Rusch DG, Greenspun DT, Allen RJ, Prince M, et al. Anatomic Imaging of Gluteal Perforator Flaps without Ionizing Radiation: Seeing Is Believing with Magnetic Resonance Angiography. J reconstr Microsurg. 2010;26:45-57.
- [10]Sung KW, Lee WJ, Yun IS, Lee DW. Reconstruction of Large Defects in the Perineal Area Using Multiple Perforator Flaps. Arch Plast Surg. 2016;43:446-450.
- [11]Lin C-T, Chang S-C, Chen S-G, Tzeng Y-S. Modification of the superior gluteal artery perforator flap for reconstruction of sacral sores. Journal of Plastic, Reconstructive & Aesthetic Surgery. 2014;67:526-532.
- [12]Geoffrey H. A Primer of Schematics to Facilitate the Design of the Preferred Muscle Perforator Flaps. Plastic and reconstructive surgery. 2009;123:1107-1115.
- [13]Kim DY, Choi HN, Park JH, Kim SR, Kim H, Han YS. Regional Analysis of Soft Tissue Thickness on Korean Buttocks and Application to Fasciocutaneous Flap Design. Arch Plast Surg. 2014;41:133-139.