Comparison of different chronic respiratory diseases in terms of cigarette smoking: A hospital-based case control study on population of Bangladesh
Abstract
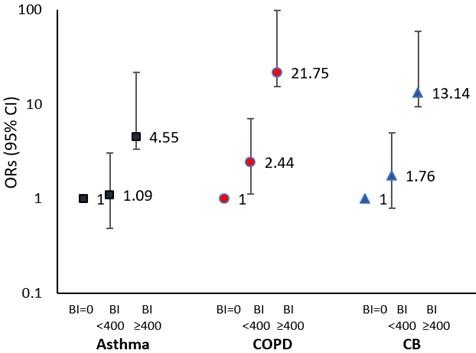
Cigarette smoking is considered as one of the main factors of developing chronic respiratory diseases (CRDs), but very few studies had been performed showing comparative association between different CRDs and cigarette smoking. This study attempts to determine and compare the association of cigarette smoking with different CRDs including chronic obstructive pulmonary disease (COPD), chronic bronchitis (CB), and asthma altogether in the context of Bangladesh. This case-control study was conducted among 406 subjects, where 297 were cases of chronic respiratory illness and 109 were controls. The diagnosis of each respiratory diseases (either asthma or CB or COPD) was confirmed by registered physicians. Of 98 COPD patients, 100 CB patients, 99 asthma patients and 109 controls, current smokers were found as 67.3%, 58%, 41.4%, and 33.9%, respectively. Current smokers with Brinkman Index (BI)≥ 400 were 43.9%, 39.7%, 26.9% and 8.2% for COPD, CB, asthma, and control group, sequentially. Regarding unadjusted association between cigarette smoking and different CRDs, current smokers with BI≥ 400 had 4.55, 21.75 and 13.14 times significantly higher chances of developing asthma, COPD and CB respectively than non-smokers. Logistic analysis revealed that after adjustment with age, body mass index (BMI) and gender, current smokers with BI≥ 400 had 6.01, 15.63 and 33.47 times more likelihood of developing asthma, CB, and COPD respectively than non-smokers; and these findings were significant as well. Thus, it can be concluded that cigarette smoking affected COPD more pronouncedly followed by CB and asthma among the study population.
INTRODUCTION
Chronic respiratory diseases (CRDs), mainly known for its long-term effects on the airways and other anatomies of the lung, include chronic bronchitis (CB), chronic obstructive pulmonary disease (COPD), asthma, emphysema, lung fibrosis etc. [1,2]. Globally 4 million people face premature death from CRDs every year [3]. Approximately, 544.9 million people had CRDs worldwide in 2017, indicating 39.8% increase from 1990 and thus became the third major cause of death [4]. This burden is higher among the low-and middle-income countries like Bangladesh where public policies to tackle the prime risk factors of CRDs are nearly absent [4].
Among all the CRDs, asthma is the most prevalent which has a direct effect to 14% of the children worldwide [5]. Around 235 million people have asthma around the globe [6] and it is rising gradually [7]. In Bangladesh, the overall prevalence of asthma was reported around 10.7% with slightly higher prevalence among the male population [8]. COPD was the second most leading cause of CRD-attributable deaths around the world in 2017, where 55.1% men and 54.8% women were suffering from it [4]. In Bangladesh, the pooled prevalence of COPD among the adult population was 12.5% [9], which is substantially higher than many countries (Malaysia, India, Hong Kong etc.) in Asia [9]. Regarding CB, the prevalence has been reported around 2.6-16% among general population in different population-based studies [10, 11] and around 7.4-53% among the COPD patients [11]. There are several risk factors of CRDs including biomass fuel usage, outdoor and indoor air pollution, occupational exposures, and so on [3, 12]. However, cigarette smoking is considered as the prime risk factors of developing COPD, asthma, and CB [7, 13, 14].
In Bangladesh, cigarette accounts for nearly half of all the tobacco smoked [15]. More than 50% of Bangladeshi men >25 years of age smoke either cigarettes or bidis [15, 16]. According to an earlier study, 172 men died of CRDs from 2003 to 2010 in Bangladesh, of which 84.9% were ever-smokers [15]. In case of COPD in Bangladesh, smoking history (both current and former) had been a significant predictor, where the duration of smoking has also been emerged an independent risk factor [15]. Furthermore, the study based on the rural community of Bangladesh showed that out of 362 current smokers, 11.6% had CB and 9.7% had asthma [17]. However, there has been no study conducted in Bangladesh showing how the effect of cigarette smoking varies among different CRDs while taking either individual or altogether into account. Therefore, this study aimed to determine and compare the association of cigarette smoking with different CRDs like COPD, CB, asthma in the context of Bangladesh.
MATERIALS AND METHODS
Study site, subjects, and procedures
This case-control study was performed among 406 subjects from December 2019 to August 2020 at the Department of Respiratory Medicine of Dhaka Medical College Hospital, Dhaka, Bangladesh. Both case and control subjects were selected randomly, and their ages were between 23 and 72 years. Data were collected based on structured close-ended questionnaire including demographic information and history of cigarette smoking. The presence of each type of respiratory illness (either asthma or CB or COPD) was confirmed through medical diagnosis performed by registered physicians; and the researchers noted that immediately at the examination room. Shortly, asthma was confirmed if the subjects showed positive bronchodilator reversibility in spirometry test, and if there was any presence of at least one asthmatic symptom (wheeze, coughing, phlegm, short breathlessness, morning cough, chest tightness, etc.) [18]. CB was defined if the subjects’ chronic chough and sputum production persisted for at least three months for two consecutive years [19]. COPD was confirmed by spirometry testing, that is when the ratio of forced expiratory volume (FEV1) to forced vital capacity (FVC) was found less than 0.70 [FEV1/FVC<0.70] at post-bronchodilator spirometry according to GOLD criteria [12]. Subjects who had asthma or CB with airways obstruction (FEV1/FVC<0.70 at post-bronchodilator spirometry) were considered as COPD in present study. Age-matched apparently healthy subjects were chosen as control who had no past history of any kind of respiratory disease.
Sample size calculation
Sample size (n) was calculated using this formula:
n= (z2 p(1-p))/d²; where:
z = Standard normal deviate at 95% confidence level
p = Prevalence of respiratory disease among the population of Bangladesh
d = Margin of error
Now, there is a variation in prevalence for different respiratory diseases of Bangladesh; like for asthma and COPD, it is 6.9% and 12.5% respectively [20, 21]. So, if z = 1.96, d = 5% =0.05, then at 95% confidence interval, sample size n becomes 98 and 168 for prevalence (p) 6.9% and 12.5% separately. However, to capture the holistic dimension of hospital going patients suffering from respiratory illness in Bangladesh, we initially thought of 250 cases in total. And adding 20% non-response, it becomes 300. So, our final cases became 297 depending on participants’ availability and consent. And approximately for every 3 cases, we found 1 control and thus we got 109 controls in total. As a result, our final sample size accumulated a total of (297 cases + 109 controls) = 406 respondents.
Ethical consideration
The study was performed according to the ethical standards of human experimentation as per Helsinki Declaration. The aim and purpose of the study were explained to the participants and written consent was taken from everyone. There was no predilection for gender, race, and ethnicity. Anonymity, confidentiality, and voluntary participation were ensured for each respondent. Participants’ safety was ensured, taking into consideration that no physical or mental stress was caused to them. The study was also approved from the institution review board, University of Dhaka (Ref. no. 89/Biol.Scs.).
Statistical analysis
Data analysis was done using SPSS program version 24 software (SPSS Inc., Chicago, USA). Categorical variables were shown in numbers and percentages. Since the data followed normal distributions; for analyzing categorical variables, Pearson’s χ2 (chi-square) test was performed and for continuous variables, student’s t-test was performed. The level of significance for each result was set at P≤0.05. All statistical tests were 2-sided. Binary logistic regression analysis was also performed to determine the adjusted associations between cigarette smoking and each type of respiratory illness.
RESULTS
Baseline characteristics of the study subjects
Among 406 subjects in total, asthma, CB, COPD and control subjects represented 24.75% (n=99), 25% (n=100), 24.5% (n=98) and 27.25% (n=109), respectively (Table 1). The mean ± SD for the age of the control group was 48.5±11.5 years; and that for the asthma, CB and COPD group were 46.9±12.4 years, 48.6±12.5 years and 49.6±11.3 years, sequentially. On the other hand, the mean ± SD for BMI of the control group was found 22.3±3.8 kg/m2; and that for the asthma, CB and COPD group were 21.6±4.1 kg/m2, 21.7±4.0 kg/m2 and 22.2±4.0 kg/m2 respectively. The proportion of female subjects was found slightly higher than male subjects in control and asthma group only. The majority of the respondents belonged to age≥ 40 years, normal BMI and primary level education for both case and control groups. No significant differences were observed regarding subjects’ age, BMI, gender and education for all groups (Table 1).
Table 1. Baseline characteristics of the study subjects.
The habit of cigarette smoking significantly differed among the study subjects
Table 2 presented cigarette smoking habit of the study subjects. Of the total 109 control subjects, 66.1% (n=72) were found with no smoking habit, whereas that for the asthma, CB and COPD group were 58.6% (n=58), 42% (n=42) and 32.7% (n=32), one by one. The Brinkman index (BI) among the current smokers was from 15 to 1000. BI≥400 was found among 8.2% of control subjects, 26.9% of asthma subjects, 39.7% of CB subjects and 43.9% of COPD subjects, and that significantly differed when compared with subjects of BI<400 (Table 2).
Table 2. Distribution of cigarette smoking habit among control, asthma, CB, and COPD subjects.
Association of cigarette smoking with asthma, CB, and COPD
To observe the association of cigarette smoking with asthma, CB and COPD, the BI of the current smokers of each respiratory disease group was divided into two categories: BI<400 and BI≥ 400 and were compared with non-smokers (BI=0) (Figure 1). It was derived from the result that current smokers with BI<400 had 1.09 times higher chance of developing asthma, 2.44 times higher chance of developing COPD and 1.76 times higher chance of developing CB than non-smokers. The risks of developing COPD and CB for the current smokers with BI<400 was also significant compared to non-smokers. On the other hand, current smokers with BI≥ 400 had 4.55 times higher chance of developing asthma, 21.75 times higher chance of developing COPD and 13.14 times higher chance of developing CB compared to non-smokers and all these differences were significant too (Figure 1).
Cigarette smoking showed significant effects on asthma, CB, and COPD after adjustments
Finally, we performed binary logistic regression analysis to observe the adjusted odds of having asthma, CB, and COPD after considering age, gender, BMI, and smoking habit (Table 3). Here, all independent variables were categorized considering age<40 years, male gender, normal BMI, and non-smokers as reference group. We found that after adjustments with age, BMI and gender, current smokers with BI<400 had increased the chance of having asthma, CB, and COPD as 1.12, 1.62 and 3.39 times higher, respectively than non-smokers. Here, only COPD vs Control group showed significance. On the other hand, after adjustments with age, BMI and gender, current smokers with BI≥ 400 had significantly increased the chance of having asthma, CB, and COPD as 6.01, 15.63 and 33.47 times higher, respectively than the non-smokers (Table 3).
Table 3. Binary logistic regression analysis.
DISCUSSION
This study illustrated the comparative association between cigarette smoking and CRDs from different gradients, which is a unique kind of study done in the perspective of Bangladesh. Bangladesh is facing an epidemic of respiratory diseases where 1,035 people die every year of COPD, and 7 million people are attacked by asthma each year [22]. So, this study is very important for addressing the comprehensive effect of smoking being one of the major risk factors of CRDs.
Our study showed that 67.3% of COPD patients, 41.4% of asthma patients and 58% of CB patients were current smokers. These findings were higher compared to previous studies [21,23.24] that showed the prevalence of COPD with current smoking habit were 24.8% in Bangladesh [23] and 18.1% in China [24]; and the prevalence of asthma patients with current smoking habit were 5.2% for male and 5.9% for female smokers [21]. On the other hand, regarding the prevalence of CB among the current smokers, our study showed similar finding to a previous study of South Korea which showed 39.45% current smokers among 127 were CB patients [25]. However, the habit of smoking stood up as a crucial predisposing factor for CRDs, for which further analysis was done to determine the dimension of its effect on various CRDs.
The present study depicted that the cumulative dose of smoking significantly related to the different CRDs. The assessment of cumulative dose of smoking was evaluated based on BI which was also performed in several studies earlier [26, 27]. According to present study, BI≥ 400 was found among 43.9%, 39.7% and 26.9% of COPD, CB, and asthma patients respectively that significantly differed than the COPD, CB and asthma patients with BI<400 respectively. Our finding was in accord with earlier studies which also showed that cumulative dose of smoking was significantly related to COPD 27 and asthma [20].
The present study also tried to determine the magnitude of association between cigarette smoking and different CRDs. Interestingly, we found that cigarette smoking had significant influence on developing asthma, COPD and CB. We showed that current smokers with BI ≥400 had 4.55, 21.75 and 13.14 times significantly higher chances of developing asthma, COPD and CB sequentially than the control subjects which supported previous Indian study [28] that showed cigarette smokers had 1.82- and 2.35 times more influence to having asthma and CB, independently than non-smokers. Thus, we can conclude that smoking habit has very good amplitude of association with CRDs, and most profoundly associated with COPD followed by CB and asthma.
Lastly, the adjusted association between cigarette smoking and CRDs was shown in the present study; and after adjusting age, BMI and gender, current smokers had significantly 6.01, 15.63 and 33.47 times more likelihood of getting asthma, CB, and COPD than non-smokers, respectively. Our findings supported previous studies where COPD was shown accounted for the adjusted ORs of 5.5 in the previously stated Bangladeshi study [21]; and as 2.63 in the Chinese study [24]. In terms of asthma, earlier study showed that current smoking habit with 15+ pack-years history had 2.37 times greater chance of developing asthma than non-smokers while adjusted for other variables 20; and for CB, the adjusted OR was significantly 1.03 in the South Korean study [25].
The present study had gone through several limitations. First, data could not be collected from hospitals of other divisions except Dhaka due to the unavailability of time and resources. Furthermore, this hospital-based study might not reflect the global picture of the whole country. But as our study site was a public hospital, so all classes of participants had been found there. Besides, most of the socio-demographic data were self-reported; there was no scope to check their authenticity. Moreover, for determining the association between cumulative dose of cigarette smoking and CRD, we considered BI< 400 and BI≥ 400 which was also considered in other study [26]. In case of some extreme poor and vulnerable people from remote areas, they might show negative attitude in most responses due to inaccessibility or unaffordability of available health facilities or commodities; anyhow, special attentions or supports were given to them during the research.
CONCLUSIONS
This study will guide to the implementation of strategies to reduce the profound effect of chronic respiratory diseases through awareness building on the harmful effects of tobacco smoking, as well as strengthening anti-tobacco policies. However, further studies are needed to fully establish the mechanism regarding the association of smoking with all kinds of chronic respiratory diseases; and thus, to mitigate the national burden of mortality from respiratory illness.
ACKNOWLEDGEMENT
Authors acknowledge the registered physician, technician and staff of the Department of Respiratory Medicine of Dhaka Medical College Hospital, Dhaka, Bangladesh for their valuable support during data collection. The authors are also thankful to the participants who gave written consent to participate in this study having confidence and trust.
AUTHOR CONTRIBUTIONS
Sumit AF and Das A were involved in the conception and design of the experiments. DAS A, Sumit AF, and Bhowmick D contributed to perform the experiments. Sumit AF analyzed data. DAS A contributed to drafting the article. DAS A and Sumit AF contributed to revising it critically for important intellectual content. Sumit AF made the final approval of the version to be published. Authorship must be limited to those who have contributed substantially to the work reported.
CONFLICTS OF INTEREST
The authors declare no conflict of interest.
References
- [1]Labaki WW, Han MK. Chronic respiratory diseases: a global view. Lancet Respir Med. 2020;8(6):531-33.
- [2]Navarro-Torné A, Vidal M, Trzaska DK, Passante L, Crisafulli A, Laang H, et al. Chronic respiratory diseases and lung cancer research: a perspective from the European Union. Eur Respir J. 2015; 46(5): 1270-80.
- [3]Khaltaev N, Axelrod S. Chronic respiratory diseases global mortality trends, treatment guidelines, life-style modifications, and air pollution: preliminary analysis. J Thorac Dis. 2019;11(6):2643-55.
- [4]Soriano JB, Kendrick PJ, Paulson KR, Gupta V, Abrams EM, Adedoyin RA, et al. Prevalence and attributable health burden of chronic respiratory diseases, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Respir Med. 2020; 8(6):585-96.
- [5]Pearce N, Aït-Khaled N, Beasley R, Mallol J, Keil U, Mitchell E, et al. Worldwide trends in the prevalence of asthma symptoms: phase III of the International Study of Asthma and Allergies in Childhood (ISAAC). Thorax. 2007; 62(9):758-66.
- [6]Kumar P, Ram U. Patterns, factors associated and morbidity burden of asthma in India. PloS One. 2017;12(10): e0185938.
- [7]Ferkol T, Schraufnagel D. The global burden of respiratory disease. Ann Am Thorac Soc. 2014; 11(3):404-6.
- [8]Mamun MM, Salauddin AS, Hossain MF, Afrin M, Asaduzzaman M, Kabir ME, et al. Prevalence of asthma and its associated factors among the undergraduate students of Bangladesh Agricultural University. Int J Nat Soc Sci. 2016;3(1):32-6.
- [9]Sutradhar I, Gupta RD, Hasan M, Wazib A, Sarker M. Prevalence and risk factors of chronic obstructive pulmonary disease in Bangladesh: a systematic review. Cureus. 2019; 11(1): e3970.
- [10]de Oca MM, Halbert RJ, Lopez MV, Perez-Padilla R, Tálamo C, Moreno D, et al. The chronic bronchitis phenotype in subjects with and without COPD: the PLATINO study. Eur Respir J. 2012; 40(1): 28–36.
- [11]Mejza F, Gnatiuc L, Buist AS, Vollmer WM, Lamprecht B, Obaseki DO, et al. Prevalence and burden of chronic bronchitis symptoms: results from the BOLD study. Eur Respir J. 2017;50(5): 1700621.
- [12]Sumit AF, Das A, Miraj IH, Bhowmick D. Association between chronic obstructive pulmonary disease (COPD) and occupational exposures: A hospital based quantitative cross-sectional study among the Bangladeshi population. PLoS One. 2020; 15(9): e0239602.
- [13]Jha P, Ramasundarahettige C, Landsman V, Rostron B, Thun M, Anderson RN, et al. 21st-century hazards of smoking and benefits of cessation in the United States. New Eng J Med. 2013; 368(4):341-50.
- [14]Varmaghani M, Farzadfar F, Sharifi F, Rashidain A, Moin M, Moradi LM, et al. Prevalence of asthma, COPD, and chronic bronchitis in Iran: a systematic review and meta-analysis. Iran J Allergy Asthma Immunol. 2016; 15(2): 93-104.
- [15]Alam DS, Jha P, Ramasundarahettige C, Streatfield PK, Niessen LW, Chowdhury MA, et al. Smoking-attributable mortality in Bangladesh: proportional mortality study. Bull World Health Organ. 2013; 91(10):757-64.
- [16]Wu F, Chen Y, Parvez F, Segers S, Argos M, Islam T, et al. A prospective study of tobacco smoking and mortality in Bangladesh. PloS One. 2013;8(3): e58516.
- [17]Sultana N, Kabir MH, Sayeed MA. Prevalence of Chronic Bronchitis, Asthma and Allergic Rhinitis in a Rural Community of Bangladesh. Chest Heart J. 2014; 38(1):11-16.
- [18]Quirt J, Hildebrand K, Mazza J, Noya F, Kim H. Asthma. Allergy Asthma Clin Immunol. 2018; 14 (Supp 2):50.
- [19]Kim V, Criner GJ. Chronic bronchitis and chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2013; 187(3):228-37.
- [20]Hassan MR, Kabir AL, Mahmud AM, Rahman F, Hossain MA, Bennoor KS, et al. Self-reported asthma symptoms in children and adults of Bangladesh: findings of the National Asthma Prevalence Study. Int J Epidemiol. 2002; 31(2):483-8.
- [21]Alam DS, Chowdhury MA, Siddiquee AT, Ahmed S, Clemens JD. Prevalence and determinants of chronic obstructive pulmonary disease (COPD) in Bangladesh. COPD. 2015; 12(6):658–67.
- [22]Bartlett E, Parr J, Lindeboom W, Khanam MA, Koehlmoos TP. Sources and prevalence of self-reported asthma diagnoses in adults in urban and rural settings of Bangladesh. Glob Public Health. 2013;8(1):79-89.
- [23]Bishwajit G, Tang S, Yaya S, Feng Z. Burden of asthma, dyspnea, and chronic cough in South Asia. Int J Chron Obstruct Pulmon Dis. 2017; 12:1093-99.
- [24]Zha Z, Leng R, Xu W, Bao H, Chen Y, Fang L, et al. Prevalence and risk factors of chronic obstructive pulmonary disease in Anhui Province, China: a population-based survey. BMC Pulm Med. 2019; 19(1):102.
- [25]Choi JY, Yoon HK, Park SJ, Park YB, Shin KC, Na JO, Yoo KH, Jung KS, Kim YK, Rhee CK. Chronic bronchitis is an independently associated factor for more symptom and high-risk groups. IntJ Chron Obstruct Pulmon Dis. 2016; 11:1335-41.
- [26]Kojima S, Sakakibara H, Motani S, Hirose K, Mizuno F, Ochiai M, et al. Incidence of chronic obstructive pulmonary disease, and the relationship between age and smoking in a Japanese population. Journal of epidemiology. 2007;17(2):54-60.
- [27]Kojima S, Sakakibara H, Motani S, Hirose K, Mizuno F, Ito M, et al. Effects of smoking and age on chronic obstructive pulmonary disease in Japan. J Epidemiol. 2005; 15(4):113-7.
- [28]Jindal SK, Aggarwal AN, Gupta D, Agarwal R, Kumar R, Kaur T, et al. Indian study on epidemiology of asthma, respiratory symptoms and chronic bronchitis in adults (INSEARCH). Int J Tuberc Lung Dis. 2012; 16(9):1270-7.