Assessment and comparison of cardiovascular disease risk factors and biochemical parameters among men and women: A cross-sectional study
Abstract
Cardiovascular disease (CVD) is one of the most common causes of death among men and women worldwide. It is predicted that by 2030 around 23.3 million people will die as a consequence of CVD. There are numerous risk factors for CVD. The goal of this study is to examine the cardiovascular clinical and biochemical parameters of hospitalized CVD patients, as well as to assess the most common risk factors. Seventy-two known healthy individuals were randomly allocated to the control group (male 47 and female 25). We collected data through a questionnaire from 154 CVD patients as a study group (male 108 and female 46). Cardiovascular status was assessed using clinical parameters like hypertension, chest pain, shortness of breathing, pain in the arm, and biochemical parameters like lipid profile, RBS, creatinine, and an electrolyte panel. Inter- and intra-group comparison was performed. A total of 154 hospitalized CVD patients were analyzed (male 108 female 46) The most significant age group for males was observed as 56-65 years (mean 60) and for females was 38-48 (mean 43) years. A highly statistically significant increase was observed in total cholesterol and LDL in males than in females, but a decrease in TG than in females. Changes were also observed in other cardiovascular biochemical and clinical parameters. There was a significant difference in smoking status, physical activity, lipid panel, and other biochemical parameters among males and females. It is concluded that studies investigating the observed sex differences in traditional risk factor effects would not only help us better understand the etiology of CVD but also help us understand how to prevent it.
INTRODUCTION
Cardiovascular disease is the leading cause of death worldwide and was responsible for an estimated 16.7 million deaths worldwide in 2010, with forecasts suggesting a startling 23.3 million by 2030. The number of deaths owing to dietary inadequacies, infectious diseases, and maternal and perinatal conditions is considered equivalent to mortality rates of CVD [1]. According to WHO, an estimated 17.9 million people died from cardiovascular diseases (CVDs) in 2019, representing 32% of all deaths worldwide. Roughly 7.4 million of these deaths (17.9 million) are thought to be caused by coronary heart disease, and 6.7 million by stroke [2]. In Europe, more than 4 million death occurred by CVD among which 49% of death occurs in women & 40% in men [3]. CVD causes more deaths in the U.S. each year than any other cause, declared to the American heart association. In the case of Asia, the central Asian countries had the highest age-adjusted mortality from CVD, followed by West Asian, South Asian, and Southeast Asian countries according to the world health organization database 2004 [4]. The populations of low- and middle-income countries like Bangladesh are increasingly being affected by CVD and account for over three-quarters of all CVD deaths [5]. Among CVDs, strokes and heart attacks are usually acute events, stroke is the second cause of death worldwide [6]. these are mainly caused by arteriosclerosis involving the heart or brain. Strokes can also be caused by blood clots or leakage from a blood vessel in the brain.
Several risk factors, such as family history, high cholesterol, high blood pressure, and being overweight or diabetic, have been linked to the development of CVD, but a significant number of people who have few or no identified risk factors will also develop CVD. Most cardiovascular diseases can be prevented by addressing behavioral risk factors, such as tobacco use, unhealthy diet and obesity, physical inactivity, harmful use of alcohol, hypertension, diabetes, and hyperlipidemia. This fact has led researchers to look for the risk factors that might be either causing CVD or that could be used to determine lifestyle changes and/or treatments that could reduce a person’s risk. People with cardiovascular disease or who are at high cardiovascular risk (due to the presence of one or more risk factors such as hypertension, diabetes, hyperlipemia, or already established disease) need early detection and management using counseling and medicines, as appropriate.
In this study, we statistically analyzed the risk factors & biochemical parameters among the patients with CVD who are hospitalized based on age, sex, smoking, diabetes, and different medical conditions. Here tried to find out any difference in biochemical parameters between males and females based on age and medical conditions and tried to identify the most common risk factors among hospitalized patients which will help to identify the disease conditions and help in the diagnosis and prognosis of the CVD.
METHODS AND MATERIALS
Institutional and ethical committee permission
For this study data were collected from hospitalized patients and outpatients through a questionnaire with written consent from Sheikh Hasina Medical, Tangail, and Chittagong Medical College, Chittagong. The study was also approved by the ethical review committee of the Department of Biochemistry and Molecular Biology, Mawlana Bhashani Science and Technology University, Santosh, Tangail-1902, Bangladesh, with the certificate number MBSTU/BMB/TEST/6/2022/152.
Study design
Subjects were divided into two groups: Group 1: Healthy control (n=72), and Group 2: patients with coronary artery disease (CAD) (n=154). The subjects in group 2 were further sub-divided into two groups; male (n=108) and female (n=46) to compare the risk factors and biochemical parameters between them.
Selection of healthy human volunteers
There were 72 healthy control (Male-47, Female-25), aged <25 to 75 years, and with BMI 18-22.9 were served healthy control. These individuals attended the outpatient department for their periodical health check-up.
Study population and data collection
Data were collected from outpatients and from the patients who were hospitalized at the ward of the coronary unit in Chittagong Medical College, Chittagong & Sheikh Hasina Medical, Tangail for this study purpose. We collected data from 154 patients (male 108 and female 46) aged between 35 to 80 with confirmed clinical diagnoses of CAD and the data included patient demographics, medical history, symptoms on arrival, results of laboratory testing, diabetes status, and smoking history, lipid-lowering medication, etc. The laboratory testing includes lipid profile, Creatinine, RBS, an electrolyte panel, and diabetes. Data were collected by using a standard questionnaire.
Determination of biochemical parameters
The biochemical parameters which were analyzed in this study were lipid profile, creatinine, random blood sugar (RBS), and electrolytes. A standard protocol was used to collect blood samples and performed the biochemical test of the blood samples for the measurement of lipid profile, creatinine level, and RBS and electrolytes.
Statistical analysis
All data were examined using IBM SPSS (Inc., Chicago, IL, USA) and Microsoft Excel. Frequency distribution, Cross-tabulation, and Bar chart were applied for the statistical estimation of the variables. Descriptive statistics like frequencies and percentages were used to determine the risk factors of CVD.
RESULTS
Demographic characteristics
The demographic characteristics such as age, weight, height, BMI, physical activity, smoking status, sleeping hours, etc. were collected from patients (Table 1).
The study population ranged in age from 25 to 75 years old (mean 60.2), with the males on average 60 years old and the females on average 43 years old. Among them 5.8% of cardiovascular patients were under the age of 25, 12.3% were 26-35 years old, 14.9 % were 36-45 years old, 18.2% were 46-55 years old, 27.9% were 56-65 years old, 13.6 % were 66-76 years old, and 7.1 % were beyond 75 years old (Figure 1). The participants range from age 56-65 and are the most susceptible to CVD in this area. This category accounts for nearly one-third of all CVD patients.
Smoking is another CVD risk factor that is attributed to the disease either directly or indirectly since it promotes plaque formation in atherosclerosis. In our study group, about 56% of patients were connected to smoking (47% of the respondents were current smokers, 9% were ex-smokers) and 44% were non-smokers (Figure 2). In the case of males 97% of patients experienced passive smoking, 63% were current smokers, 10.2%were ex-smoker, and 26.9% never did smoke. On the other side, 43.5% of female patients experienced passive smoking, 10.7% were current smokers, 4.3% were ex-smoker and 84.8% were a non-smoker (Table 1).
CVD patients’ physical activity, such as the morning or other sorts of modest exercise was observed. Between males and females, a substantial difference in physical activity patterns was observed. A total of 17% of males and 27% of females never performed any type of physical activity. Physical activity was performed frequently by 48% of males and 39% of females, compared to occasionally by 35% of males and 34% of females (Figure 3). Females are more likely than their male counterparts to have never exercised.
The average sleeping hours of CVD patients were also investigated, with 20.8 percent of patients sleeping for 0-4 hours, 36.4 percent for 4-5 hours, and 42.86 percent for 6-7 hours (Table 1).
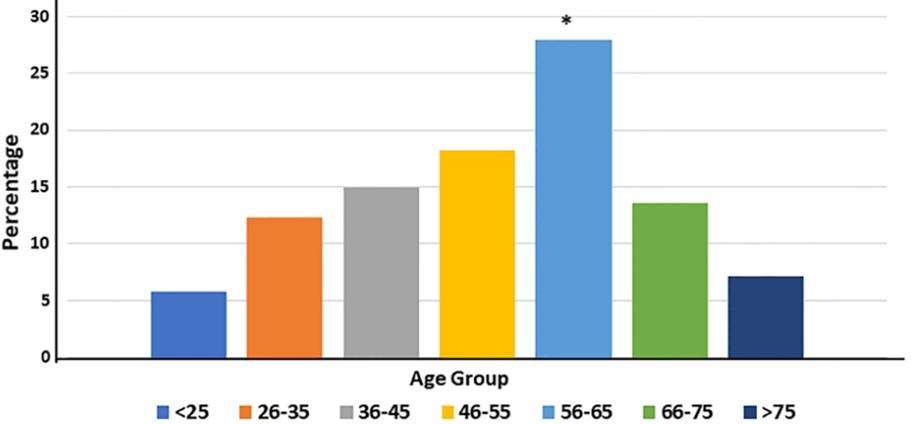
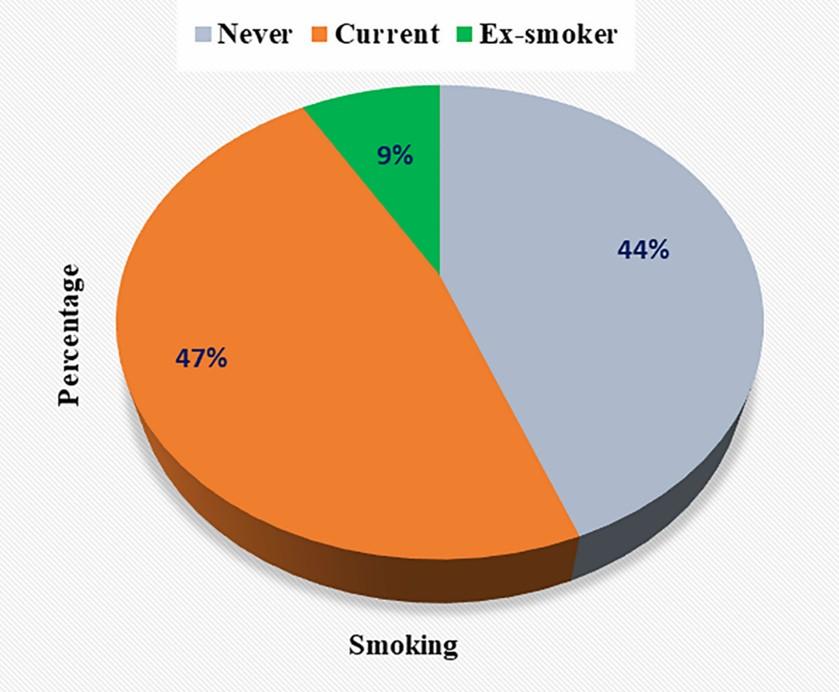
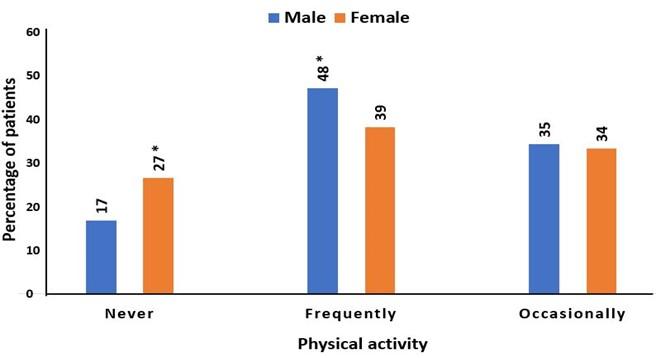
Table 1. Demographic profile and medical history of the participants.
Medical history
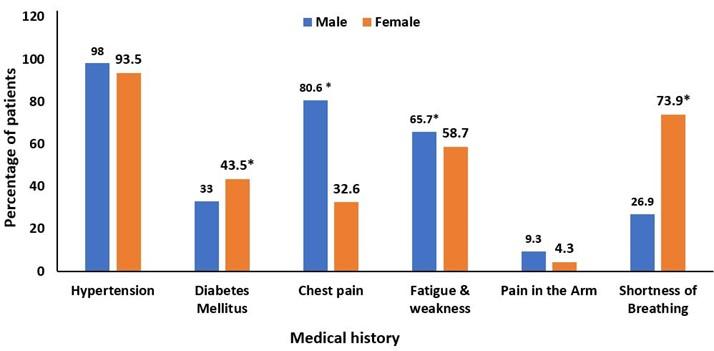
Males and females in the study group had their medical histories examined for hypertension, chest pain, diabetes mellitus, fatigue and weakness, and arm pain, shortness of breathing. Among males 98% of patients had hypertension, 33% had diabetes mellitus, 80.6% had chest pain, 65.7% felt fatigued and weak, 9.3% experienced pain in the arm and, 26.9% experienced shortness of breathing. On the contrary, among females 93.5% of patients had hypertension, 43.5% had diabetes mellitus, 32.6% had chest pain, 58.7% experienced fatigue and weakness, 4.3% felt pain in the arm and, 73.9% felt shortness of breathing. Hypertension was the most common medical symptom in both males (98%) and females (93.5%), with males having a higher rate than females. The number of patients with diabetes mellitus is greater in females (43.5%) than in males (33%) (Figure 4).
Cardiovascular biochemical parameters
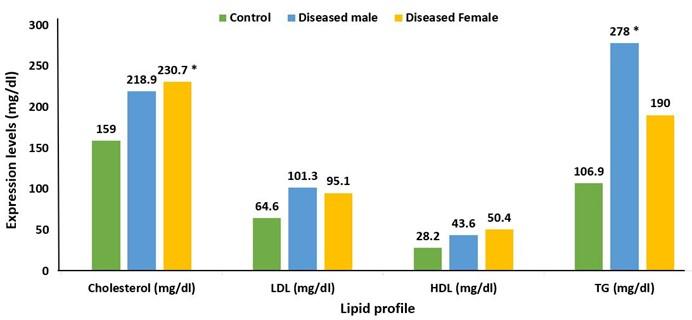
Lipid profile, creatinine, random blood sugar (RBS), and electrolyte level were the biochemical parameters examined in this study. The lipid profile such as total cholesterol, low-density lipoprotein (LDL), high-density lipoprotein (HDL), and TG of diseased males and females compared with that of control. The mean value of LDL, HDL, TG, and total cholesterol of diseased persons was higher than that of the control. The mean value of total cholesterol and HDL was higher in females (230.7 and 50.4) than that in males (218.9 and 43.6). LDL and TG mean values are greater in males (101.3 and 278) than in females (95.1 and 190) (Figure 5).
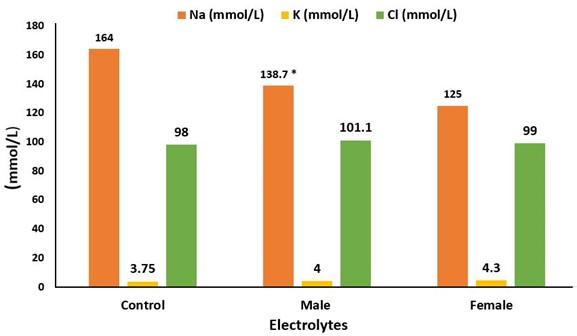
We compared the electrolyte level of the control group with that of diseased males and females. The diseased group had an imbalanced level of electrolyte value compared to the control group. Diseased males (138.7) and females (125) both had a lower mean value of Na than the control group (164). But the mean value of K and Cl of the control group (3.75 and 98) was slightly lower than that of the diseased male (101.1 and 4) and female (99 and 4.3) (Figure 6).
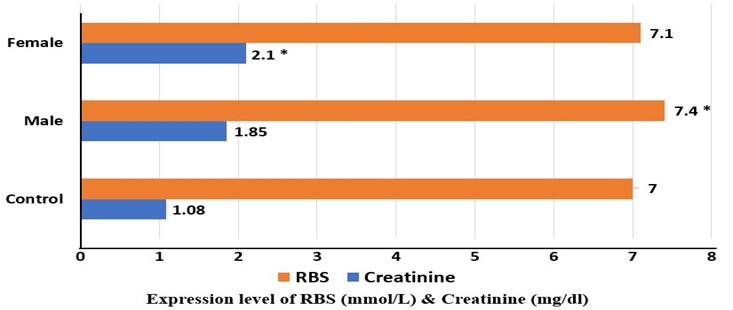
The creatinine and RBS level of the patients was also analyzed. The creatinine level of the diseased group was higher than that of the control group (1.08), where the female (2.1) had a higher creatinine mean value than that of the male (1.85). In the case of RBS, both diseased males (7.4) and females (7.1) had a higher mean value of RBS than that of the control group (7). Among the diseased group, the males had a slightly higher mean value of RBS than females (Figure 7).
DISCUSSION
Cardiovascular disease is one of the leading causes of death both in males and females worldwide. The majority of the burden of CVD is explained by a group of classic risk factors which influence both men and women, such as high blood pressure, smoking, being overweight or obese, diabetes, and high cholesterol [7]. In this study, we tried to find out the risk factors associated with cardiovascular disease in patients who are hospitalized. We analyzed the demographic profile and biochemical parameters of the patients.
The most important risk factor influencing cardiovascular homeostasis is age [8]. As a consequence, one-fifth of the world’s population will be 65 or older by 2030, resulting in an exponential rise in the prevalence of CVD due to an additional 27 thousand individuals with hypertension, 8 million with coronary heart disease, 4 million with stroke, and 3 million with heart failure [9]. In our study, we found the age group 56-65 is most vulnerable to CVD, more than one-fourth (27.9%) of the patients belonged to this age group. Approximately 13% of patients were in the age group 26-35, 15% were in the age group 36-45, 18.2% of the patients were in the age group 45-55 and 13.6% were in the age group 66-75. Around 75% of the patient’s ages were greater than 35 years old, CVD can be an old men’s disease. In our study, the mean age of CVD for males is 60 years and for a female is 43.6.
Smoking is another risk factor for CVD patients. According to epidemiological studies, cigarette smoking (CS) increases the risk of myocardial infarction (MI) and fatal CAD in both men and women [10,11]. Low-tar cigarettes and smokeless tobacco have been proven to enhance the risk of cardiovascular events in smokers compared to non-smokers. [12]. Even passive smoking (atmospheric tobacco exposure) with a smoke exposure one-hundredth that of active CS is correlated to a 30% increase in CAD risk, compared to an 80% increase in active smokers [13]. In our study, we found approximately 56% of the patients were connected to smoking, and 75 % of males and 15% of females were connected to smoking. Among whole patients, 47% were current smokers and 9% were ex-smokers. 81% of all patients were passive smokers where 97% were male, and 43% were female (table 1). Around 90% of whole hospitalized CVD patients (49% current, 9% ex-smoker, 27.9% passive smokers) were connected to smoking
Physical inactivity and a less active lifestyle have been linked to significant increases in CVD risk. Elimination of a sedentary lifestyle may reduce CVD by 15% to 39% and stroke by 33% [14]. Physical activity like morning walks, running, walking, and other shorts of exercise can reduce the risk of CVD. In our study group, 27% of females and 17% of males never did physical exercise. More males (48%) did exercise frequently than females (39%).
The most common medical conditions of CVD patients were hypertension, fatigue & weakness, diabetes mellitus, and shortness of breathing. Hypertension was most common among males and females. The prevalence of hypertension is broadly similar in men and women and is projected to increase with population growth and aging in both sexes. In 2000, nearly a billion adults, 27% of all men and 26% of all women, had hypertension; these estimates are projected to increase to 1.5 billion adults, 29% of men, and 30% of women, in 2025 [15]. In our study, the number of females (93.5%) with hypertension was lower than males (98%). More males experienced fatigue & weakness (65.7%) than females (58.7%), on the contrary, more females (73.9%) experienced shortness of breathing than males (26.9%).
Total cholesterol and LDL are key modifiable risk factors for atherosclerotic vascular disease and its clinical symptoms, according to several studies. The ratio of HDL to total cholesterol was thought to be a principal determinant of the sex difference in CHD risk. [16]. Prospective epidemiological data have suggested that the relationship between LDL and CHD is log-linear, with a relative risk set at 1.0 for LDL of 40 mg/dL [17]. In the present study, almost 80% of patients hospitalized with CAD have total cholesterol, LDL, and TG higher than that of the control group. The mean value of total cholesterol and LDL was higher in males than females, but HDL and TG were lower in females.
The electrolyte imbalance is related to CVD; especially K imbalance is one of the causes of a heart attack. In our study, diseased males (138.7) and females (125) both had a lower mean value of Na than the control group (164). Males had higher mean values of Na and K than females, whereas females had higher mean values of Cl than males.
Both RBS and creatinine level was greater in the diseased group than that in the control group. The mean value of creatinine was higher in females (2.1) than males (1.85), but the mean RBS value was lower in females (7.1) than males (7.4)
CONCLUSIONS
Cardiovascular diseases remain the world’s leading cause of death and disability in both men and women but affect more women than men. The conventional risk factors account for the majority of the CVD burden. While the effects of high blood pressure, obesity, and cholesterol on cardiovascular outcomes are largely similar in men and women, long-term smoking and diabetes are much more dangerous for women. More research into the studies investigating the observed sex differences in traditional risk factor effects would not only help us better understand the etiology of CVD but would also help us understand how to prevent it. It is equally critical that women and medical professionals are aware of these disparities to lower the risk of CVD.
ACKNOWLEDGEMENTS
The authors would like to express their gratitude to the authorities of Sheikh Hasina Medical College, Tangail, and Chittagong Medical College, Chittagong, as well as the entire study population for their enthusiastic engagement. This work was supported by grants of Research Cell, MBSTU from the University Grants Commission of Bangladesh and, the Ministry of Science and Technology, Bangladesh.
AUTHOR CONTRIBUTIONS
MJI was involved in the conception and design of the study. AI and FAN were involved in data collection, analysis, and interpretation of data. SI and SS contributed to the analysis and manuscript writing. MJI and SS revised it critically for important intellectual content.
CONFLICTS OF INTEREST
There is no conflict of interest among the authors.
References
- [1]Bansilal S, Castellano JM, Fuster V. Global burden of CVD: Focus on secondary prevention of cardiovascular disease. Int J Cardiol 2015;201:S1–7.
- [2]Hajar R. Framingham Contribution to Cardiovascular Disease. Heart Views 2016;17:78–81.
- [3]Tsioufis C. Cardiovascular disease statistics: The Greek reality. Hell J Cardiol 2018;59:301–2.
- [4]Ohira T, Iso H. Cardiovascular disease epidemiology in Asia – An overview. Circ J 2013;77:1646–52.
- [5]Laslett LJ, Alagona P, Clark BA, Drozda JP, Saldivar F, Wilson SR, et al. The worldwide environment of cardiovascular disease: Prevalence, diagnosis, therapy, and policy issues: A report from the American college of cardiology. J Am Coll Cardiol 2012;60:S1–49.
- [6]Avan A, Digaleh H, Di Napoli M, Stranges S, Behrouz R, Shojaeianbabaei G, et al. Socioeconomic status and stroke incidence, prevalence, mortality, and worldwide burden: An ecological analysis from the Global Burden of Disease Study 2017. BMC Med 2019;17.
- [7]Appelman Y, van Rijn BB, ten Haaf ME, Boersma E, Peters SAE. Sex differences in cardiovascular risk factors and disease prevention. Atherosclerosis 2014;241:211–8.
- [8]Kovacic JC, Moreno P, Nabel EG, Hachinski V, Fuster V. Cellular senescence, vascular disease, and aging: Part 2 of a 2-part review: Clinical vascular disease in the elderly. Circulation 2011;123:1900–10.
- [9]Nichols M, Townsend N, Scarborough P, Rayner M. Cardiovascular disease in Europe 2014: Epidemiological update. Eur Heart J 2014;35:2950–9.
- [10]Jonas MA, Oates JA, Ockene JK, Hennekens CH. Statement on smoking and cardiovascular disease for health care professionals. Circulation 1992;86:1664–9.
- [11]Ambrose JA, Barua RS. The pathophysiology of cigarette smoking and cardiovascular disease: An update. J Am Coll Cardiol 2004;43:1731–7.
- [12]Negri E, Franzosi MG, La Vecchia C, Santoro L, Nobili A, Tognoni G. Tar yield of cigarettes and risk of acute myocardial infarction. Br Med J 1993;306:1567–70.
- [13]Glantz SA, Parmley WW. Passive Smoking and Heart Disease: Mechanisms and Risk. JAMA J Am Med Assoc 1995;273:1047–53.
- [14]Giada F, Biffi A, Agostoni P, Anedda A, Belardinelli R, Carlon R, et al. Exercise prescription for the prevention and treatment of cardiovascular diseases: part I. J Cardiovasc Med (Hagerstown) 2008;9:529–44.
- [15]Kearney PM, Whelton M, Reynolds K, Whelton PK, He J. Worldwide prevalence of hypertension: a systematic review. J Hypertens 2004;22:11–9.
- [16]Hada DS, Garg S, Ramteke GB, Ratre MS. Effect of Non-Surgical Periodontal Treatment on Clinical and Biochemical Risk Markers of Cardiovascular Disease: A Randomized Trial. J Periodontol 2015;86:1201–11.
- [17]Sachdeva A, Cannon CP, Deedwania PC, Labresh KA. Lipid levels in patients hospitalized with coronary artery disease : An analysis of 136, 905 hospitalizations in getting With The Guidelines 2009.