Study on assessment of reproductive hormones in male patients with type 1 and 2 diabetes mellitus
Abstract
The process and viability of fertility are affected by diabetes mellitus, which is also associated with hyperglycemia. Males who experience hypogonadism or anxiety may find it difficult to feel sexually exhilarated. The aim of the present study is to assess reproductive hormone levels in type 1 diabetes mellitus (T1DM) and type 2 diabetes mellitus (T2DM) male patients. This study included 79 healthy controls and 158 male patients with T1DM and T2DM between the ages of 20 and 49 years. Levels of reproductive hormones such as follicle-stimulating hormone (FSH), luteinizing hormone (LH), testosterone (T), and prolactin (PRL) were measured. The results showed notable variations in the levels of these hormones among patients of different ages. PRL levels were significantly elevated in T1DM compared to T2DM in the age groups of 20-29 and 30-39. FSH and LH levels in all age groups were greatly increased in T1DM compared to T2DM, but T hormone levels were dramatically reduced in T1DM patients compared to T2DM patients. Additionally, patients with a disease duration of 11–15 years demonstrated a significant decrease in T hormone compared to those with a disease duration of 1–5 years. Because of age-related variations in hormone levels between T1DM and T2DM as well as a decline in T hormone levels over the course of the disease, high levels of PRL hormone may therefore exacerbate the effects of diabetes, which in turn may influence the reproductive hormones.
INTRODUCTION
A metabolic disorder with numerous etiologies known as "diabetes" is defined by persistent hyperglycemia and abnormalities in the metabolism of protein, lipid, and carbohydrate brought on by deficits in insulin synthesis, insulin action, or both [1]. It is estimated that 380 million people globally have diabetes, with 8.3 percent prevalence rate [2]. Insulin shortage results from type 1 diabetes mellitus (T1DM), a long-term autoimmune condition with a significant inflammatory component that is brought on by the loss of pancreatic beta cells that produce insulin in the Langerhans Islands [3]. However, insulin resistance and comparatively low insulin production are features of type 2 diabetes mellitus (T2DM) [4]. The primary causes of type 2 diabetes are thought to be genetics and dietary practices. It is well known that stress, poor diet, inactivity, and obesity all have a major impact on T2DM [5, 6]. Numerous organs, including pot retinopathy, which may cause vision loss; nephropathy, which may cause renal failure; Charcot joints; peripheral neuropathy, which may cause foot ulcers and amputation; and autonomic neuropathy, which may result in symptoms of the gastrointestinal and urogenital systems, cardiovascular issues, and sexual dysfunction, can all suffer long-term damage, imbalances, and failure as a result of diabetes [7].
Although the bulk of diabetes-related problems have been exhaustively researched, reproductive system anomalies are a subject of little knowledge [8]. In fact, diabetes is linked to sexual dysfunction in both genders. Impotence, ejaculatory disorders, decreased libido, reduced lubrication of the vagina, and orgasmic disorders are among the pathophysiologic conditions that are thought to involve neuropathy, vascular insufficiency, and psychological problems [8, 9]. T1DM has been observed to be linked to decreased sperm viability, motility, and vitality in the ejaculate [10]. However, it is yet unknown if variations in the levels of reproductive hormones are related to male infertility [11]. Prolactin (PLR) is the most fundamental hormone, which regulates reproductive well-being. Diabetic patients with erectile dysfunction exhibited lower testosterone levels than people without diabetes [12]. Additionally, changes in insulin synthesis may affect how well the testicles and auxiliary glands operate [13].
Thus, the aim of the present study is to assess reproductive hormone levels in T1DM and T2DM male patients based on age and disease duration.
MATERIALS AND METHODS
Ethical approval
The Maysan Health Department/Al-Sadr General Hospital in the province of Maysan authorized a committee to approve the current study by obtaining the informed consent of all participants (Approval number: 2017-02).
Design of study
Between 2017 and 2018, the study was carried out in the Al-Sadr Teaching Hospital in the province of Maysan. In the current study, 158 male patients with diabetes mellitus (DM) between the ages of 20 and 49 were recruited, 85 of whom had T1DM and 73 had T2DM. The control group consisted of 79 males who appeared to be in good health. The patients were separated into three age groups: 20-29 years, 30–39 years, and 40–49 years, as well as three periods, such as (1–5), (6–10), and (11–15) years, according to the duration of the disease.
Blood samples collection
Blood samples were collected in the morning (8–10 am) in a volume of blood to limit the daily variance in hormone levels (5 cc). The samples were centrifuged to separate them after being allowed to coagulate at room temperature for 15 minutes (3000 cycles for 5 minutes). Before measuring the levels of reproductive hormone, PRL serum is kept in a refrigerator at -20 oC.
Biochemical assays
Serum levels of testosterone (T), luteinizing hormone (LH), and follicle-stimulating hormone (FSH) and PRL hormones were measured for patients and healthy control groups by using commercial kits (BioMerieux, Askim, Sweden) according to the manufacturer's instructions. Briefly, the ingredients were taken out to come to room temperature (about 30 minutes). For every sample, control, or calibrator that needs to be tested, and one "reproductive hormones or PRL" strip and one "reproductive hormones or PRL" solid-phase receptacle (SPR) were used. The "reproductive hormones or PRL" code on the device served as identification for the test. The reproductive hormones or PRL calibrator (S1) was used to identify the calibrator. The control of reproductive hormones or PRL was recognized by (C1). The vortex mixer was used to mix the calibrator, control, and sample of serum separated from the pellet. 200 µl is the amount used for the calibrator, control, and sample test. Finally, SPRs and reproductive hormones, or PRL reagent strips, were inserted in the correct positions on the device.
Statistical analysis
The data were statistically analyzed using SPSS version 19 and an independent t-test. For more than two independent means, a one-way ANOVA was applied. The data of the current study were presented as a mean ± standard error of the mean. (P < 0.05) was identified as statistically significant between the groups.
RESULTS
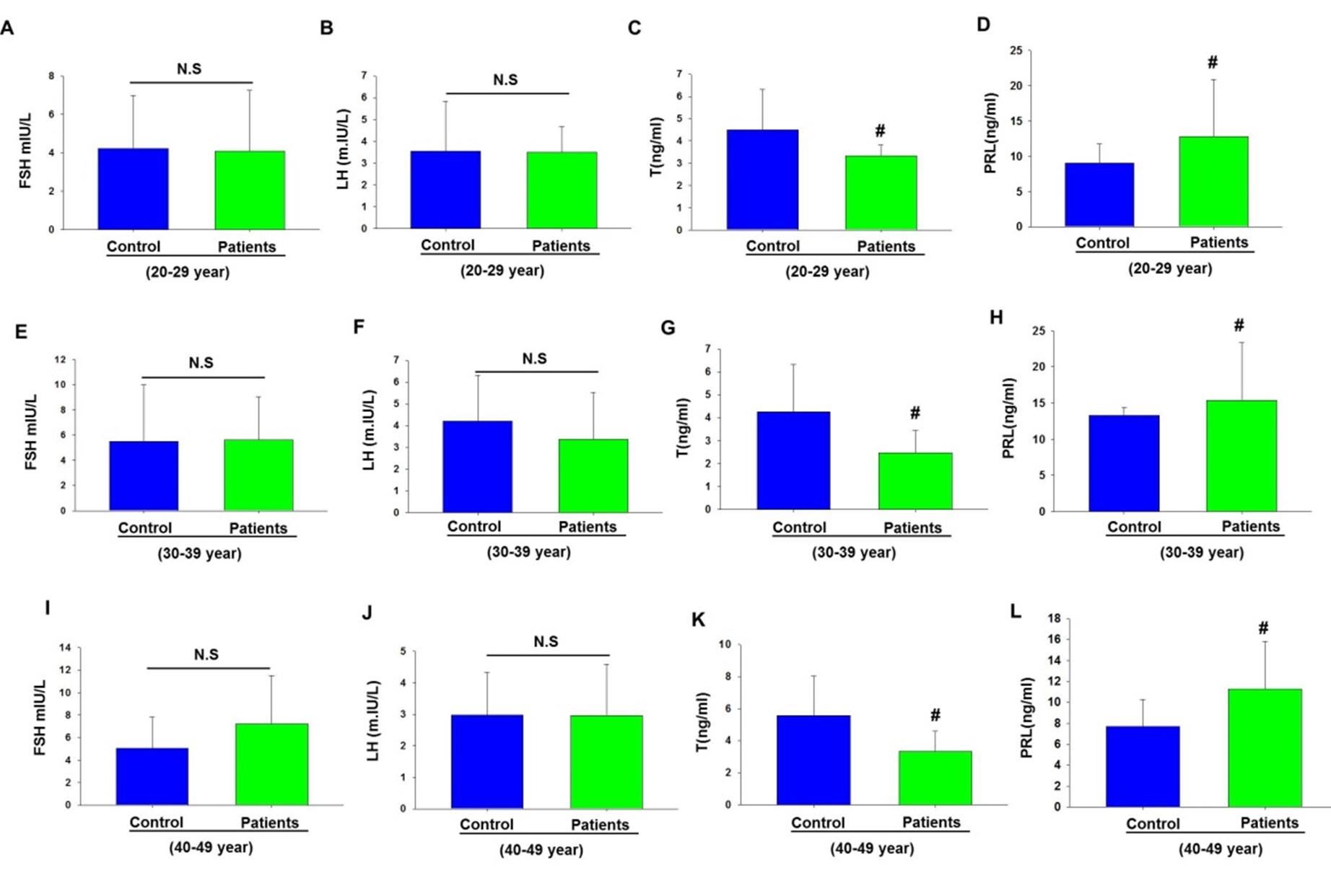
Levels of reproductive hormones in T1DM male patients
Insulin resistance has been shown to affect the hypothalamus, pituitary, gonads, and perigonads. As a result, less gonadal steroids such as T, LH and FSH are secreted [14]. PLR also regulates reproductive health. In the present study, we examined reproductive hormone levels in T1DM patients and also in healthy control groups in three age groups. Our findings revealed that the levels of T were significantly decreased in T1DM patients in all age groups as compared to control groups (Figure 1 C, G, and K). The results also observed a substantial increase in the levels of PRL in the serum of patients with T1DM compared to control groups (Figure 1D, H, and L). However, the statistical analysis observed no significant differences in the FSH and LH levels as compared to healthy control groups (Figure 1A, B, E, F, I, and J).
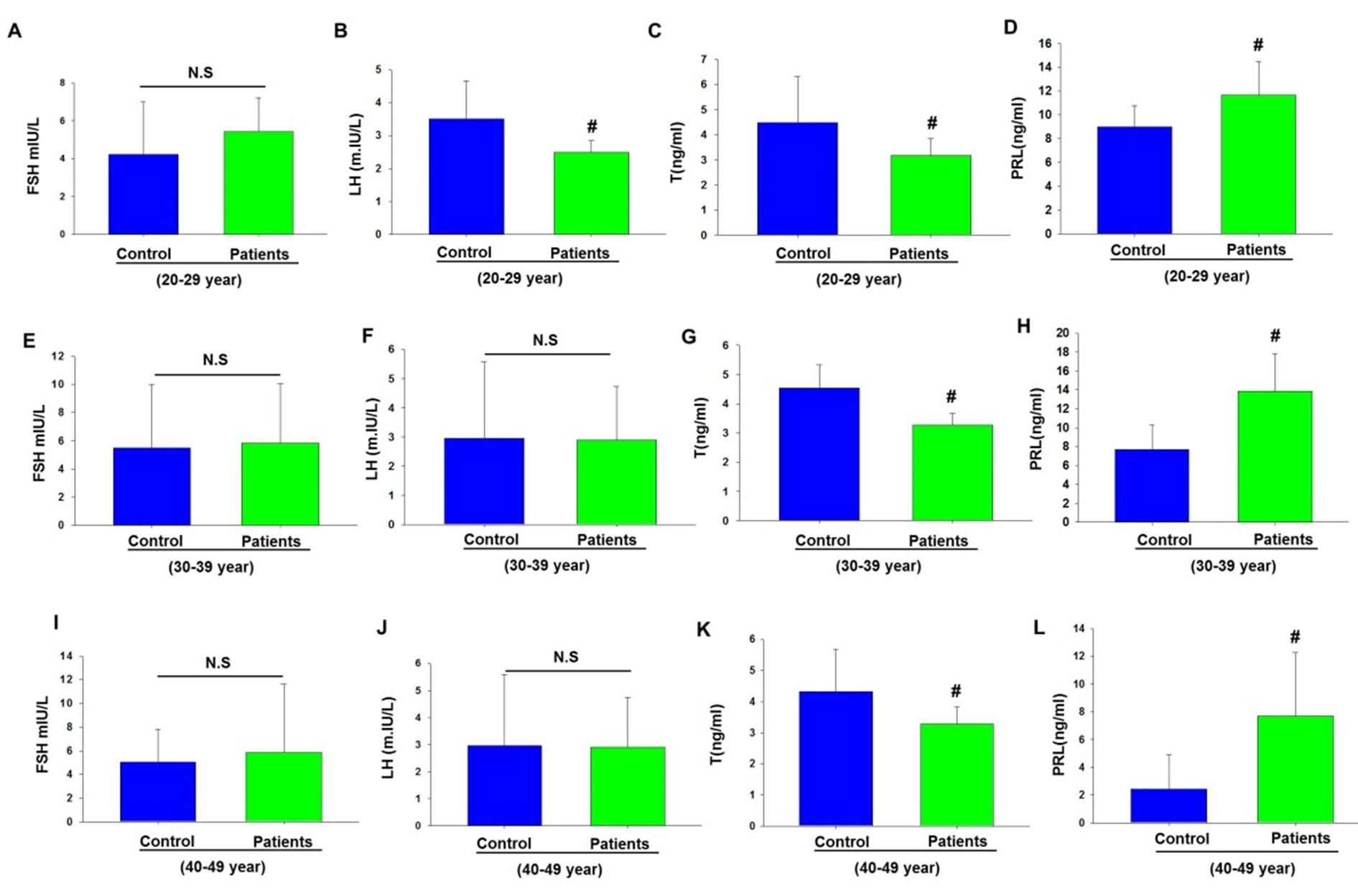
Levels of reproductive hormones in T2DM male patients
Next, we explored the reproductive hormones and PRL levels in the serum of patients with T2DM and in healthy individuals (Figure 2). Our results found that there are no significant differences in the levels of FSH in T2DM patients as compared to control groups (Figure 2A, B, E, F, I and J). Notably, we found that the levels of LH and T hormones significantly decreased (p<0.05) in the serum of patients with T2DM, corresponding to the levels of T in healthy groups (Figure 2C, G, and K). Whereas our finding observed that the levels of PRL were greatly increased in the serum of patients with T2DM compared to healthy controls (Figure 2D, H, and L).
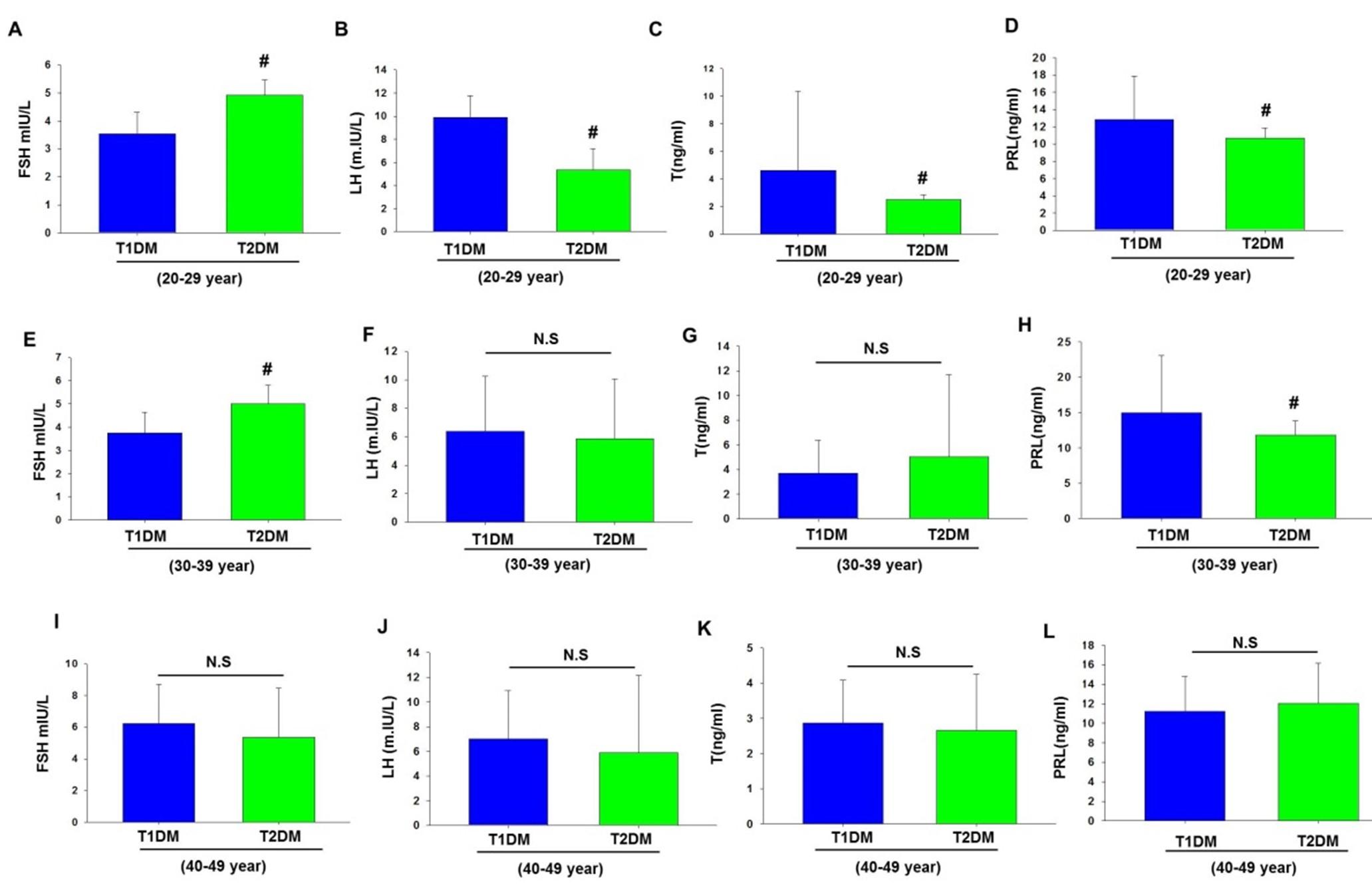
Comparison of reproductive hormones in T1DM and T2DM male patients
It was interesting to estimate the levels of reproductive hormones and PRL in the serum of both T1DM and T2DM male patients. The statistical analysis showed a significant increase in the levels of FSH of patients with T2DM in relation to the levels of FSH of T1DM patients in the age group (20-29 years) (Figure 3A). While the LH, T, and PRL levels of T2DM male patients were significantly reduced compared to the levels of LH, T, and PRL of T1DM patients (Figure 3B, C, and D). Moreover, the results also found a substantial increase in the levels of FSH in patients with T2DM in the age group (30-39) years as compared to T1DM patients with the same age group (Figure 3A). Notably, the statistical analysis showed no significant differences in the levels of LH and T between T1DM and T2DM patients in the age group (30-39) years (Figure 3B and C). However, the results observed a significant decrease in the levels of PRL of patients with T2DM as compared to the levels of PRL of T1DM patients in age group (30-39) years (Figure 3D). Additionally, our results found no substantial differences in FSH, LH, T, and PRL levels in the serum of T1DM and T2DM patients that fall in the age group (40-49) years (Figure 3I, J, K, and L).
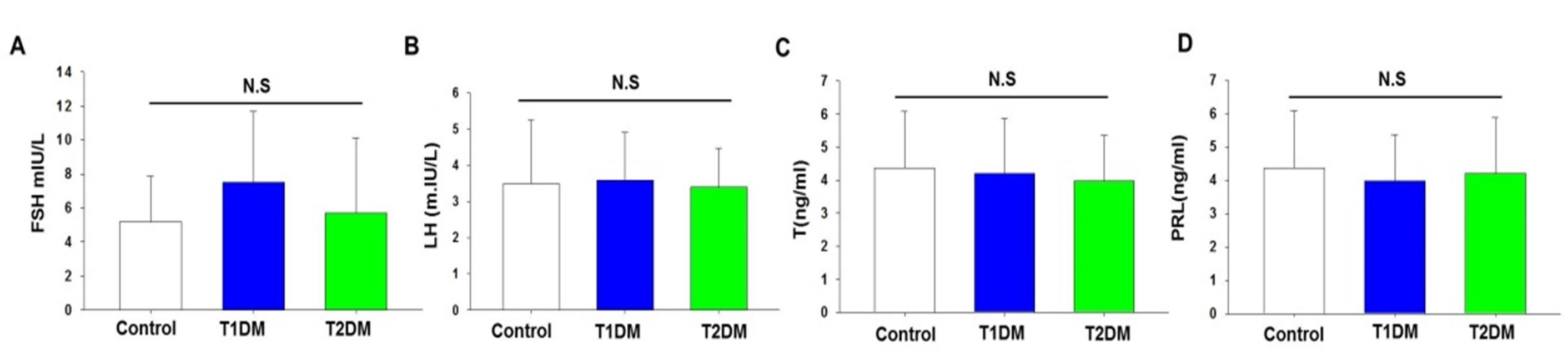
Levels of reproductive hormones in T1DM and T2DM male patients regardless of age
It was important to examine reproductive hormones and RL hormone levels in T1DM and T2DM male patients, regardless of age. In terms of reproductive hormone and PRL levels, the statistical analysis revealed no significant differences between T1DM, T2DM patients and healthy control groups, and corresponding to p-values of 0.22, 0.91,0.18 and 0.07, respectively (Figure 4A, B, C, and D).
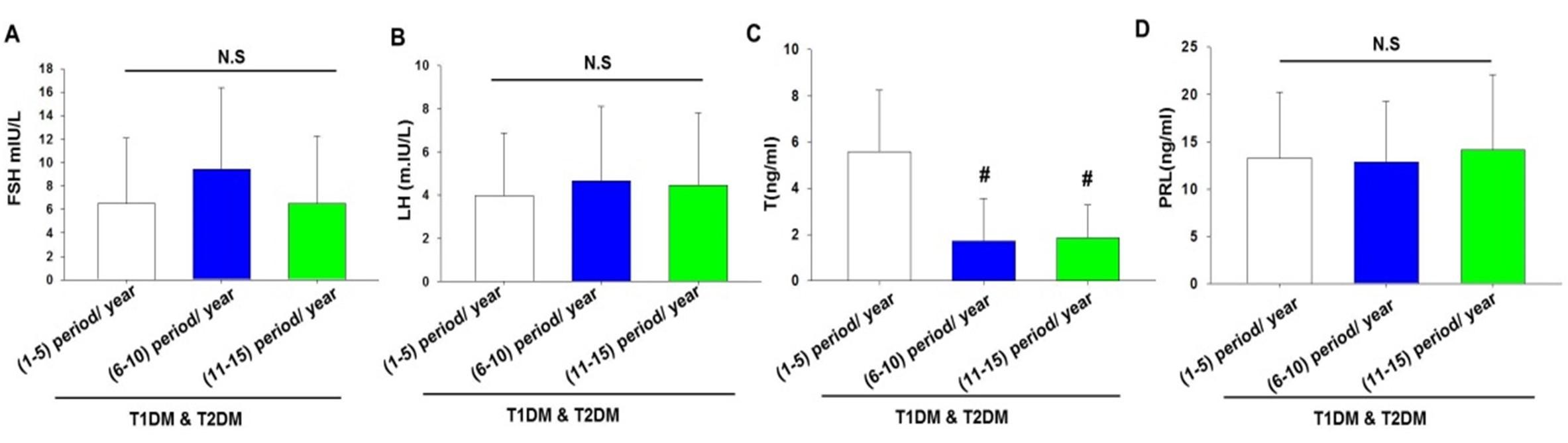
Levels of reproductive hormones in T1DM and T2DM male patients according to period of disease
Next, we examined the reproductive hormones and PRL hormone levels in patients with T1DM and T2DM based on how long the disease has been present (Figure 5). The results found that there are no appreciable variations in the levels of FSH, LH, and PRL between healthy control groups and those with T1DM or T2DM patients, and according to the period time (1-5, 6-10, and 11-15, respectively) (Figure 5A-D).While we found that the levels of (T) were substantially decreased by 3-fold and 2.8-fold in the duration period (6-10 and 11-15), respectively, relative to the control group (Figure 5C).
DISCUSSION
Diabetes is a serious metabolic disease that can cause a number of issues, including problems with men's reproductive systems. Diabetes in men has been linked to lower-quality semen and impaired reproductive function [14, 15]. Our findings have revealed that the levels of T were substantially decreased in both T1DM and T2DM male patients. Additionally, the present results found that PRL levels were greatly elevated in male patients with T1DM and T2DM. Thus, regulating PRL hormone and insulin resistance could enhance the reproductive function of males with T1DM and T2DM.
A recent study has shown that the hypothalamus, pituitary gland, and gonads can all be affected by insulin deficiency or its resistance. Subsequently, gonadal steroids like FSH, LH, and testosterone are secreted less as a result of this condition [16]. In the present study, we found that male patients with T1DM and T2DM had substantial decreases in the levels of T hormones compared to healthy individuals. It is important to mention here that our findings were in line with previous studies showing the effect of insulin resistance on male fertility [11, 17, 18]. In fact, T hormone levels could also be decreased in diabetic males by aromatase enzymes via the conversion process of testosterone into estradiol in adipose tissue [19]. It was found that the ratio of total testosterone to estradiol can be used as an indicator for T2DM [20]. A previous study demonstrated that 33% of T2DM male patients showed a great reduction in the free levels of T hormone [21]. Moreover, previous findings have shown that insulin resistance might be behind the decreased number of Leydig cells which in turn affects the concentration of T hormones [22, 23]. Insulin has been demonstrated to play a significant role in regulating the pituitary and gonad functions [24]. Oxidative stress can also affect how well the hypothalamus and pituitary operate normally in diabetic patients [25]. It is believed that LH secretion controls the production of testosterone, and blood testosterone levels reflect the health of the hypothalamic-pituitary-gonadal axis. As a result, decreased testosterone levels associated with insulin-dependent diabetes may point to a malfunction at one or more functional levels of the hypothalamus pituitary-gonadal axis [11].
High levels of PRL hormone synthesis may indeed play a major role in the onset of diabetes. For instance, recent studies have found that elevated levels of PRL hormones can impair the sensitivity of insulin and increase the progression of insulin resistance [26-29]. Our findings observed a significant increase in the levels of PRL hormone in male patients with T1DM. Moreover, the present results also found that the levels of PRL hormone were significantly increased in male patients with T2DM. Our findings suggested that high levels of PRL hormone might greatly participate in the induction of insulin resistance and diabetes development, and this condition could affect male reproductive function. In fact, further studies are needed to explore the role of PRL in the reproductive function of diabetic male patients.
CONCLUSION
Our findings demonstrated that T1DM and T2DM could greatly affect reproductive hormones. The results found that the levels of the T hormone were substantially decreased in both T1DM and T2DM male patients. Furthermore, our findings revealed that male patients with T1DM and T2DM had significantly elevated levels of PRL hormone. The present findings suggest that the high levels of PRL hormone might affect the fertility of males by increasing the progression of insulin resistance, which in turn decreases the levels of T hormone.
ACKNOWLEDGEMENTS
We acknowledge Al-Sadr General Hospital in Mysan for their assistance in providing samples and for granting us permission to use their lab equipment. Finally, we would like to express our gratitude to the Amara Technical Institute, College of Science, University of Misan, and Biology Department for their technical assistance.
AUTHORS CONTRIBUTION
The writing and interpretation of the results were assisted by NAH, RM, ZAJRA, AAS, and HK. The study was developed, planned, and some of the writing was done by RM. All authors gave their approval to the final manuscript.
CONFLICTS OF INTEREST
There is no conflict of interest among the authors.
References
- [1]Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: Diagnosis and classification of diabetes mellitus provisional report of a who consultation. Diabet Med. 1998;15:539-53.
- [2]Guariguata L, Whiting DR, et al. Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res Clin Pract. 2014;103:137-49.
- [3]Eizirik DL, Colli ML, et al. The role of inflammation in insulitis and beta-cell loss in type 1 diabetes. Nat Rev Endocrinol. 2009;5:219-26.
- [4]Butler AE, Janson J, et al. Beta-cell deficit and increased beta-cell apoptosis in humans with type 2 diabetes. Diabetes. 2003;52:102-10.
- [5]Kahn SE, Hull RL, et al. Mechanisms linking obesity to insulin resistance and type 2 diabetes. Nature. 2006;444:840-6.
- [6]Riserus U, Willett WC, et al. Dietary fats and prevention of type 2 diabetes. Prog Lipid Res. 2009;48:44-51.
- [7]American Diabetes A. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010;33 Suppl 1:S62-9.
- [8]Zarzycki W, Zieniewicz M. Reproductive disturbances in type 1 diabetic women. Neuro Endocrinol Lett. 2005;26:733-8.
- [9]De Berardis G, Pellegrini F, et al. Clinical and psychological predictors of incidence of self-reported erectile dysfunction in patients with type 2 diabetes. J Urol. 2007;177:252-7.
- [10]Miralles-Garcia JM, Garcia-Diez LC. Specific aspects of erectile dysfunction in endocrinology. Int J Impot Res. 2004;16 Suppl 2:S10-2.
- [11]Ballester J, Munoz MC, et al. Insulin-dependent diabetes affects testicular function by fsh- and lh-linked mechanisms. J Androl. 2004;25:706-19.
- [12]Bhasin S, Enzlin P, et al. Sexual dysfunction in men and women with endocrine disorders. Lancet. 2007;369:597-611.
- [13]Chandrashekar V, Bartke A. The impact of altered insulin-like growth factor-i secretion on the neuroendocrine and testicular functions. Minerva Ginecol. 2005;57:87-97.
- [14]Andlib N, Sajad M, et al. Abnormalities in sex hormones and sexual dysfunction in males with diabetes mellitus: A mechanistic insight. Acta Histochem. 2023;125:151974.
- [15]Cree-Green M, Newcomer BR, et al. Peripheral insulin resistance in obese girls with hyperandrogenism is related to oxidative phosphorylation and elevated serum free fatty acids. Am J Physiol Endocrinol Metab. 2015;308:E726-33.
- [16]Schoeller EL, Schon S, et al. The effects of type 1 diabetes on the hypothalamic, pituitary and testes axis. Cell Tissue Res. 2012;349:839-47.
- [17]Cheung KK, Luk AO, et al. Testosterone level in men with type 2 diabetes mellitus and related metabolic effects: A review of current evidence. J Diabetes Investig. 2015;6:112-23.
- [18]Hofny ER, Ali ME, et al. Semen parameters and hormonal profile in obese fertile and infertile males. Fertil Steril. 2010;94:581-4.
- [19]Kelly DM, Jones TH. Testosterone: A metabolic hormone in health and disease. J Endocrinol. 2013;217:R25-45.
- [20]Olasore HSA, Oyedeji TA, et al. Relationship between testosterone-estradiol ratio and some anthropometric and metabolic parameters among nigerian men. Metabol Open. 2023;18:100249.
- [21]Dhindsa S, Prabhakar S, et al. Frequent occurrence of hypogonadotropic hypogonadism in type 2 diabetes. J Clin Endocrinol Metab. 2004;89:5462-8.
- [22]Ali BR, Alameri AN, et al. Correlation between reproductive hormones levels and semen quality in patients with diabetes. J Med Life. 2022;15:1507-10.
- [23]Pitteloud N, Hardin M, et al. Increasing insulin resistance is associated with a decrease in leydig cell testosterone secretion in men. J Clin Endocrinol Metab. 2005;90:2636-41.
- [24]Baccetti B, La Marca A, et al. Insulin-dependent diabetes in men is associated with hypothalamo-pituitary derangement and with impairment in semen quality. Hum Reprod. 2002;17:2673-7.
- [25]Muriach M, Flores-Bellver M, et al. Diabetes and the brain: Oxidative stress, inflammation, and autophagy. Oxid Med Cell Longev. 2014;2014:102158.
- [26]Bahceci M, Tuzcu A, et al. Is hyperprolactinemia associated with insulin resistance in non-obese patients with polycystic ovary syndrome? J Endocrinol Invest. 2003;26:655-9.
- [27]Tuzcu A, Yalaki S, et al. Evaluation of insulin sensitivity in hyperprolactinemic subjects by euglycemic hyperinsulinemic clamp technique. Pituitary. 2009;12:330-4.
- [28]Peric B, Kruljac I, et al. Obesity and hypercholesterolemia in patients with prolactinomas: Could dhea-s and growth hormone be the missing link? Endocr Res. 2016;41:200-6.
- [29]Yang H, Lin J, et al. Prolactin is associated with insulin resistance and beta-cell dysfunction in infertile women with polycystic ovary syndrome. Front Endocrinol (Lausanne). 2021;12:571229.