Management of mental health during COVID-19 pandemic: possible strategies
Abstract
In the 21st century, any pandemic, especially, SARS-CoV-2 is a global burden due to high incidence, mortality, and mutation rate. Although several techniques have already been identified to control the pandemic or treat patients and causes of adverse impact on mental health, relatively only, fewer researchers have little concern about finding effective mitigation strategies to improve mental health. Therefore, this study aimed to find some common and unique approaches to manage mental health during a pandemic. Some strategies for the better management of mental health induced by SARS-CoV-2 infections are required for all classes of peoples. Early management is vital, and those must be associated with frontline workers and people staying at home, particularly in isolation centers and already identified as active cases. Experts have pointed out the need to pay specific attention to proper daily life. To manage abnormal mental conditions, such as anxiety, mood, personality, and psychotic disorder during the pandemic; social media, meditation, and psychological motivation with adequate diet, exercise, and sleep have significant roles in regulating some biological mechanism, incredibly immune, hormonal, and neural process. Management of mental health is mandatory for all at the time of the SARS-CoV-2 pandemic. We can consider all of the strategies mentioned above to treat mental health during and after the COVID-19 pandemic condition.
INTRODUCTION
The outbreak of SARS-CoV-2 is considered both epidemic and pandemic in the world. Currently, people all over the world have been affected by SARS-CoV-2, which is the fifth pandemic after the 1918 flu pandemic [1]. COVID-19 is turning into COVID-21 by crossing COVID-20, but infections and death are increasing with generating several problems. The outbreak caused by SARS-CoV-2 likely to cause an increase in global issues like economic burden, poor healthcare infrastructure [2], social issues, [3] political problems, hunger or malnourishment, and lastly, the most magnitude is the mental health problem in both developed and developing countries [4, 5]. Accumulating evidence suggests that SARS‐CoV‐2 mediated outbreak can damage psychological or mental health during a pandemic which is not something new as people have faced a similar crisis in the past year for every pandemic like the Ebola virus disease outbreak [6], SARS, MERS [7] influenza outbreak [8, 9]. Longtime epidemics can negatively impact people in several ways, such as feelings of personal danger of infection, concern for relatives as well as family [10]. Furthermore, losing jobs, decreased earnings, unpayable loans due to low income are indicative causes of mental stress [11]. Shammi (2020) reported that longtime lockdown leads to unemployment, demotion, and hunger problem due to the food shortage of poor people that ultimately contribute to panic and mental stress in people [12]. Zhai and Du (2020) conclude that inadequate healthcare facilities in some countries, i.e., limited testing that is also confined to the urban area and inadequate treatment facilities, negatively impact public mental health [13]. A recent study by Magson et al. summarized that COVID-19 related worries, teething troubles of learning online, and raised family disagreement were also associated with the greater psychological problem [14]. Widespread rumors and misinformation in social media and indirect exposure to continuous news may have had a wide variety of psychological effects, including stress-related disorders [15]. Moreover, some additional factors, including inadequate material supplies, businesses failure, travel shut down, mutation of the virus, and conflicting vaccination, may also cause psychological problems. As a consequence, these factors may trigger feelings of anger, anxiety, grief, loneliness, boredom and may lead to severe mental health problem [16, 17]. Moreover, this mental health crisis may also increase other problems like xenophobia, suicide, heart problem, insomnia, stroke, chronic pain, threatening behavior, erratic or unusual behavior, self-injury, paranoid thinking, and drug addiction among the people [18, 19]. The previous studies conclude that pandemic induced mental problems result in post-traumatic stress disorder (PTSD) symptoms, including nightmares, hyperarousal, detachment, numbing, and the risk of infections such as pneumonia [20, 21]. The meta-Analysis by Pappa et al. amalgamated thirteen studies with a total of 33,062 participants and reported that 12 reviews were anxiety positive which is accounted for 23·2%, whereas depression was consistent in 10 studies, with an incidence rate of 22·85% [22]. Insomnia was another prominent mental health issue with having an incidence rate of 38·9% per 5 reports by the same author. Furthermore, descriptive analyzes have been performed and found that 18.7% of the sample revealed depressive behavior, 21.6% anxiety, and 15.8% PTSD symptoms [23]. Data about mental health status caused by SARS-CoV-2 is available globally, but the proposed mechanism for managing this mental health-related problem is rare. It may be due to lack of available information. Therefore, in this review, the authors proposed few possible strategies to manage mental health during COVID-19 pandemic.
MANAGEMENT OF MENTAL HEALTH DURING COVID -19 PANDEMIC
Psychological distress, i.e., insomnia, alcohol/drug misuse, and symptoms of posttraumatic stress disorder (PTSD), depression, anxiety, burnout, anger, and higher perceived stress, are normal during disasters like the COVID-19 pandemic. People, particularly doctors as well as other health care practitioners (hospital staff members, receptionists, cleaners, and caterers), are susceptible to the adverse effects of psychological disorders because they seek to balance the responsibility of caring for patients, their families, and friends. It’s essential to improve people’s mental and physical well-being to minimize distress and slow the occurrence of serious problems such as depression or anxiety. There are good evidence-based guidelines in this section that can reduce the negative impact and promote well-being. Following are the possible ways to manage mental health during this pandemic.
Exercise
The COVID-19 pandemic made people fixed at home (isolation and quarantine), and physical and social activity was decreased which led to increased emotional or behavioral disorders like fear, terror, depression, anxiety. The results from previous performed observational and experimental studies demonstrated that regular physical exercise could suggestively progress mental health and reduce depression, nervousness, and stress symptoms [24-29].
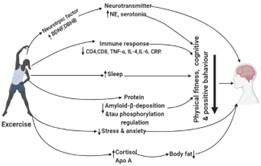
In recent research on physical activity, physical exercise is recommended for both indoors and outdoors people during the COVID-19 outbreak as it is beneficial for boosting up the immune system to relieve anxiety and depression [29-32]. Studies have shown that several types of exercise effectively lower blood pressure, enhance cardiovascular health, and prevent various cancers, as well as diabetes, osteoporosis, hypertension, obesity, and Alzheimer’s disease [25-28]. Studies on animal models have also shown that exercise positively affects depression by controlling neurotransmitters, neurogenesis, neurotrophic factors, and cerebral blood flow. In vivo experiment conducted by Sleiman SF et, al. reported that exercise is a factor that appears to raise the amount of brain-derived neurotrophic factor (BDNF) in the hippocampus, which is shown to combat sadness and anxiety in mice by storing an endogenous molecule, D-β-hydroxybutyrate (DBHB). Besides, regular physical activity will reduce BDNF levels and provide neuroprotection and neurotrophic impact in a similar model [33]. A study from Gokdemir et al. and Daniele et al. reported that exercise could help increase norepinephrine (NE) levels and serotonin metabolites in the mouse brain to prevent depressive behavior and neurochemical shift. [34, 35].
Long-term research carried out by Wu et al. on TgF344-AD transgenic, and wild rats concluded that exercise reduced anxious-depressed behaviors and enhanced fear-preventing action by controlling amyloid-β-deposition, hyperphosphorylation, microgliosis, inflammatory cytokines release, and oxidative damage [24]. A clinical study in twenty-one participants by Passos et al. summarized that long-term moderate aerobic exercise training improved sleep, lowered depression and cortisol, and enhanced significant changes in immunologic variables like increased plasma apolipoprotein A and decreased CD4 and CD8 [36]. In another study, Woods et al. summed up that routine exercise protects against neural diseases such as dementia and depression through potential pathways including weight loss, declines in macrophage accumulation in adipose tissue, macrophage modifications, exercise-induced muscle development of IL-6, for the effect of anti-inflammatory activities [37]. Exercise is compared to antidepressant medication as a first-line treatment for mild to moderate depression. For instance, animal models show that daily aerobic activity improves brain serotonergic and noradrenergic levels similar to antidepressants effects. [38]. Anxiety is the most prevalent type of mental illness, causing disturbed sleep, mood changes, and difficulty completing ordinary tasks [39]. Vogelzangs and Michopoulos reported that exercise could regulate pro-inflammatory cytokines and C-reactive protein (CRP) via the inflammatory response, which improves anxiety symptoms [40]. A study conducted by China on college students showed that regular physical activity could alleviate stress and anxiety induced by COVID-19 or improve mental health behavior [5]. Adlard et al. reported that physical activity was found to accumulate BDNF at pre-stress levels, meaning that the exercise protects from stress-related lower BDNF levels [41]. Furthermore, a recent study stated that relaxation and breathing strategies were recommended as potential measures to improve sleep quality, anxiety, and depression in COVID-19 patients [42].
According to Liu et al., the anxiolytic effect is due to enhancing hippocampal neurogenesis and restoring neurotransmission of neuropeptide Y (NPY), while Lopresti et al. described in his literature that exercise helped to up-regulate hypothalamic-pituitary-adrenal (HPA) axis in animal- and human-based studies [43, 44]. Exercise can help to minimize inflammation and lead to improved mental health outcomes for patients with inflammatory disorders. For instance, a study in eighty patients by Abd El-Kader et al. showed that exercise might minimize inflammation through reducing necrosis factor-alpha (TNF-α), interleukin-4 (IL-4), interleukin-6 (IL-6), and C-reactive protein (CRP) [45]. In a meta-analysis study by Heyn et al., exercise results in older people with cognitive disability and dementia showed that practice instruction increases fitness, physical performance, cognitive function, and constructive actions [46].
Keeping mentally and physically active during the COVID-19 outbreak will help reduce the negative impact on mental health following the COVID- plague. As a whole, further investigation is needed to prove the efficiency of exercise as a first-line or active treatment. But we all can agree that exercise is an effective way of decreasing stress, depression, and anxiety based on the data and previous research. Overall, exercise can be a therapeutic way to manage mental health-related disorders during an emergency situation, depicted in Figure 1.
Diet
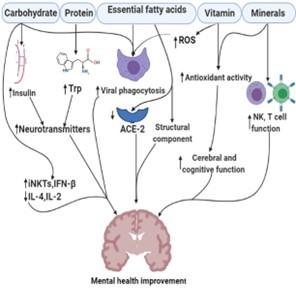
A proper diet during the COVID-19 pandemic is vital. Although no food or nutritional supplements can prevent infection with SARS-CoV-2, good diets are essential to promote immune systems and improve psychological conduct. According to the World Health Organization (WHO), eating healthy, frozen, and unrefined foods every day to get the body’s needs in terms of vitamins, minerals, dietary fiber, protein, and antioxidants is also a safe way with better immune systems and a minor risk of chronic conditions and infectious illnesses [47]. This section provides scientific information and evidence on the importance of food and bioactive ingredients in health management.
Carbohydrate
Carbohydrate intake induces insulin release into the body, and this insulin can cause blood sugar to enter cells to provides energy, activates tryptophan into the brain, and affects neurotransmitter levels [48].
Rao et al. reported that water-soluble polysaccharides and the complexes of polysaccharide proteins might enhance and trigger immune responses in macrophages and activate the system by binding the natural killer T-cells (iNKTs) on antigen cells to CD1 receptors. Furthermore, carbohydrate is capable of inhibiting inflammation by reducing IL-4, IL-6, CRP production while increasing IFN-β production [49].
Rodríguez-Valentín et al. reported in their in vitro study that mushroom polysaccharides were associated with anti-HIV activity through suppressed virus replication and upregulation of some antiviral chemokines, including macrophage inflammatory protein (MIP-1α/β) and stromal cell-derived factor-1 alpha (SDF-1α) [50]. Some carbohydrates significantly impact memory development during short, stressful times by releasing cortisol [51]. Several studies have shown that carbohydrate consumption enhances the ability to focus, response speed, processing ability, mood, and memory, while disturbances in carbohydrates raise the risk of cognitive memory disorders [52]. Randomized Controlled Trial by Owen et al. suggests that higher carbohydrate doses can affect memory in both hippocampal and non-hippocampal brain regions [53]. A systematic review conducted by Hoyland (2009) summarized that eating a regular breakfast or consuming glucose can help enhance mental efficiency by increasing memory effectiveness with attention task capability than no breakfast group [54]. Clinical data suggest that a low glycaemic index (GI) breakfast allows healthier cognitive activities in rats and humans [55].
Protein
Dietary protein and individual amino acids like tryptophan and tyrosine consumption help improve cognitive development and brain function discussed in observational and interventional studies by van de Rest (2013) [56]. High-quality protein foods (meats, milk, and others, eggs) improve the brain’s functioning and mental health by producing neurotransmitters like dopamine and serotonin from amino acid tyrosine and tryptophan [48]. An experimental study conducted by Khaliq et al. reported that a high dose of tryptophan (50 -100 mg/kg) and serotonin or their metabolites improve cognitive performance in the bred albino Wister rats (150-160 g) model [57]. Based on a previous study, it can be suggested that foods rich in protein can help manage mental health induced by the SARS-CoV-2 infection; also, WHO suggests that consuming protein from animal sources, including fish, meat, milk, and eggs as high calorie and high protein diets are considered necessary to prevent or attenuate the loss of lean muscle in COVID-19 patients [58]. In a study, Muscogiuri et al. highlighted that protein-rich foods such as milk, yoghurt, seeds, and nuts could be a better source of tryptophan (an amino acid and serotonin precursor) during the quarantine period of COVID-19 to manage mental health [59].
Essential fatty acids
The fundamental role of fat in immunity has been established in the literature; for instance, monounsaturated and polyunsaturated fatty acids have a beneficial immune modulated impact. [60]. These bioactive lipids also exhibit macrophage phagocytic ability and have a beneficial effect in treating a viral infection [61]. There are a lot of essential fatty acids, like omega-6 and omega-3, may be effective in preventing and controlling SARS-CoV-2 infection and other enveloped viruses with inhibiting angiotensin-converting enzymes (ACE, an ACE-2 precursor), decreasing the supply of SARS-CoV-2 receptors and subsequently making unable to reach the target cell [62, 63]. Furthermore, in vivo studies in the patients suspected of being COVID- 19 showed that lipids including fatty acids, phytosterols, and carotenoids improve immune response, anti-inflammatory activity, decrease the risk of cardiovascular disease by inhibiting ACE 4 receptors as well as limiting virus ability to reach cells [64, 65].
The omega-3 fatty acids, especially alpha-linolenic acid (ALA), are essential for the brain’s structure and function. It’s been assumed that sufficient polyunsaturated fatty acids (PUFAs), especially Docosahexaenoic acid (DHA), inhibit the development of depression [48].
Vitamin
Vitamin is a crucial participant in the army of immunity. Carr et al. conclude that vitamin supplements can benefit those vulnerable to respiratory virus infections; for example, vitamin C is a potent source of antioxidants and caused reactive oxygen species (ROS) mediated phagocytosis and chemo taxis to destroy the viral pathogen [66]. The main comorbidities of COVID-19 patients are common cold, diabetics, cardiovascular, kidney, cancer, the microbial infection can be prevented with the help of consuming antioxidant vitamin C through promoting immune functions, autophagy inducing, and reducing inflammation and oxidative stress by lowering NF-kB, CRP, and ILs [67]. McCartney et al. reported that vitamin D shortage is thought to down regulate cluster of differentiation 2 (CD26), interleukin-6 (IL-6), and interferon-gamma (IFNγ) those are considered molecule for COVID-19 host cell defense system [68]. Baksi et al. confirmed that severe vitamin D shortage in young rats could elevate catecholamine levels in the brain [69]. Furthermore, a study conducted by Benton et al., supplementation of nine B-complex vitamins especially, vitamin B2 and B6 status, ten times over standard recommended dietary allowance (RDA) for the 1-year improved mood in both men and women [70]. Clinical studies have shown that vitamin B12 prevents the onset of dementia symptoms. The addition of cobalamin stimulates older people’s brain and cognitive functions; It also supports frontal lobe factors [71]. During the COVID-19 pandemic, sufficient zinc and vitamin C and D intake may be a promising pharmacological tool for preventing starting the inflammatory process [72].
Minerals
Minerals are essential micronutrients used in DNA synthesis and cell proliferation, regulating both innate and adaptive immune systems like the production of immune cells [73]. Velthuis et al. reported that increasing the intracellular zinc with pyrithione can be a potential inhibitor for RNA viruses replication as well as SARS coronavirus (SARS‐CoV) at low concentrations [74]. Furthermore, Golub et al., summarized from some of the experimental animal (rodents, monkeys, human) study, have shown clearly that Zinc deficiency, mainly at the time of pregnancy, leading the loss of neurons and reduced brain volume [75]. Selenium is a significant mineral and has important roles in the humoral system through the antioxidant mechanism to induce NK cell and leukocyte function [76]. Copper is an essential trace element that can prevent scavenger free-radical and builds up at inflammatory sites, which is important for IL-2 production [77, 78]. Furthermore, it can help T cell proliferation, antibody production and maintain immunity [78, 79]. The iodine helps to energy metabolism in the cerebral cell, and iodine deficiency at the time of pregnancy induces severe cerebral malfunction resulted in cretinism [80].
Dietary phytochemicals
Phytochemicals use anti-SARS agents due to the ability to inhibit several mechanisms either at the viral entry point or the replication stages or via immunomodulation potentials [81]. Honey is a significant phytochemicals source, and its mechanisms of anti-viral properties and its very vast and unknown [82]. Abedi et al. summarized that honey and its main components inhibit the entry of the virus into the host cell and its replication and modulate the inflammatory cascade [83]. Islam et al. summarized in their literature review that several phytochemicals from N. sativa could be an alternative therapy to combat SARS-CoV-2 infection [84] through induction of IL‐8 [85], increasing CD4+ T and IFN‐γ number with activities [86]. A recent clinical study with 200 patients showed that Nigella sativa administration recovered patients from COVID-19 related symptoms [87]. The curcumin-based placebo-controlled trial was carried out on COVID-19 patients and revealed that curcumin reduces the inflammatory markers, i.e., IFN-γ, IL-17, Il-4, TGF-β, GATA-3, t-bet, ROR- γT, and FoxP3to of COVID-19 patients [88]. In a clinical study with melatonin (hormone-like compound and COVID-19 patients found that melatonin increased the recovery rate through reducing oxygen saturation, significant symptoms, and improvement of tumor necrosis factor-alpha (TNF-ɑ), cytokines like C-reactive protein (CRP), 1β IL-1β, and interleukin- IL-6 within ranging seven days of randomization [89]. Similarly, several other phytochemicals are continuously testing to treat COVID-19 patients. In summary, the possible beneficial role of diet against mental health caused by SARS-CoV-2 is indicated in Figure 2.
Sleep
Psychological distress and signs of mental illness are associated with severe outbreaks of COVID-19 infections [90]. Scientists, on the whole, are trying to manage mental health-related disorders caused by COVID-19, where proper sleep can be a significant candidate. Recent studies outlined by Franceschini et al. (2020) suggest that central Italian people who died due to COVID-19 dramatically altered sleep-wake patterns marked by usual early or delayed bedtime average faster waking time decreased naps in the afternoon [91]. According to the world health organization (WHO), they recommended that people in isolation take regular sleep routines to manage mental health [92]. Melatonin is a pineal hormone that responds to darkness during sleep time, and recent studies outlined by Zhang et al. (2020) suggest that melatonin supports critical care patients in the COVID-19 pandemic by reducing anxiety and improving sleep quality [94, 95]. Sleep regulates major antioxidants enzyme-like catalase, glutathione peroxidase, and accumulation of reactive oxygen species (ROS) of oxidative stress-associated disease [96, 97]. Mirmiran et al. in their in vitro study, found that sleep deprivation can decrease brain mass, neuronal cell death, and increase the risk of eventual behavioral problems during development [98], while proper sleep or rapid eye movement (REM) sleep is required in neonate for appropriate neural development termed the ontogenetic REM sleep hypothesis [99]. The synaptic homeostasis hypothesis (SHY) proposed by sleep researchers, where sleep is thought to reduce synaptic strength between neurons and sleep promote synaptic weakening. This will help to recover energy stores and relieve cellular stress [100].
Sleep has a direct impact on the maintenance of immunity and the immunological response linked to the psychological problems imposed by COVID-19. Milrad et al. demonstrate that pro-inflammatory molecules, including interleukin (IL-1ꞵ, IL-6), TNF-α, and CRP, raised due to poor sleep in people, and a higher level of pro-inflammatory cytokines causes called “cytokine storm” related to mortality in COVID-19 patients [93, 94]. Crosstalk between sleep and immune system by Besedovsky et al. reported that sleep less than 6 hours declines the level of T lymphocytes, the activity of natural killer cells (NK), and shorter telomere length of T-cells and sleep disturbance is associated with a decline in response to vaccines leading to increase susceptibility to infectious diseases. [95, 96]. Lallukka, T. & Sivertsen (2017) summarized that insomnia therapy has potential roles in improving general mental health [105], so sleep improvement might help manage and prevent mental health disorders. Teker (2017) reported that sleep deprivation is linked to increased anxiety, whereas better sleep quality is connected to decreased stress and anxiety through improving psychosocial support [106]. Random sampling from 240 schools children aged 6-11 years of Nahavand city in Iran and found that sleep dysfunction is closely correlated with the psychological issue of their mental health problem, but sleeping education for parents and school trainers will help to boost the children’s mental health by reforming proper sleep patterns [107]. Ojio (2016) has estimated that the night sleep period correlated with the lowest risk of depression/anxiety for teenagers aged 7-12. For men, the lowest depression/anxiety may be related to sleeping 8.5 h or more, while for females, the period was reported at 7.5 h or more [108]. An observational study with a total of 2,631 participants by Supartini et al. demonstrated that depressive symptoms and eventually suicidal ideation are linked with low sleep quality, while enhancing the standard of sleep will avoid the occurrence of depression and decrease the risk of suicide [109].
Motivations
Motivation is the psychological counselling that encourages someone to work on a problem; those are the direct link to stress and physical health while enlightening individuals’ activity in a work context [102-105]. So motivations can be an alternative therapy and may become an adjunctive for the management and treatment of the mental health of COVID-19 infected patients by SARS-CoV-2. Motivation is essential for the quarantine people, possible symptoms of suspected case and positive case so that these people keep feet in mentally during the pandemic. The best motivation during a pandemic is that people believe that maintaining quarantine and social distance interventions, including home-stay, have been introduced worldwide to minimize virus transmission [114]. The WHO recommended that motivation from knowing about fact and clear evidence about reducing the risk of infection is needed to manage mental health. Furthermore, they suggested getting motivated from regular contact with beloved ones through e-mail, social media, telephone, or video conference to manage mental health induced by SARS-CoV-2 infections [92]. Self-confidence is an immune-modifying psychotherapeutic intervention that can potentially benefit COVID-19 patients. Hannan et al. summarized that improving self-confidence through multiple ways like social supports, psychological interventions, food habits, spiritual connections, health supports, and positive thinking can potentially suppress psychological stress, thereby consolidating immune functions. Furthermore, they also report that self-motivation can help improve non-communicable diseases such as neurodegenerative and inflammatory bowel diseases. Consequently, self-confidence enables an individual to overcome COVID-19 and reduces the risk of contracting the disease [93]. Firth et al. summarized in their review, professional support has the capability to tackle psychological barriers by improving physical activity [115]. Motivation can help change our thinking, feeling, and behaving, whereas lack of motivation suppresses functioning and well-being. Simpson and Balsam suggest that motivation can be an alternative way to treat several psychological and neurological disorders through improving the endocrine system, circadian system, neurotransmitter function [116]. During a pandemic, impulsive motivation increases student learning capacity by creating a neural network between the motivation (reward) and the brain memory systems. Rodgers summarized that motivation itself, as well as its complex role, can help to regulate behavior change and maintenance in a critical situation [117]. A well-motivated person can help others like suspected to consume a balanced diet, proper sleep, and regularly perform a physical exercise; those will help to mitigate the mental health-related problems during the pandemic crisis. Although the higher incidence rate in the COVID-19 compared to the previous pandemic, the case fertility rate is rare with a higher recovery rate. So, it should not be panic and worried about the ongoing pandemics.
Social media
SARS-CoV-2 infections turned the world into uncertainty, and the continuous news from social media about the severity of coronavirus infection and mortality rate made people in a puzzle. This kind of information negatively impacts people’s mental health [20, 110, 111]. According to some research, social media can be a definite cause of depression. For instance, I. Pantic (2014) summarized that prolonged use of social networking sites (SNS), such as Facebook, may be related to signs and symptoms of depression [14]. But being alarmed about the COVID-19 related news is understandable; individuals can handle current mental health issues, such as limiting the information and being concerned about what one has read, listening to, and seeing. Anyone may feel nervous or upset by a nearly continuous influx of news stories concerning an epidemic. During some hours of the day, check out health providers for detailed alerts and realistic advice to avoid sharing infection-related rumors responsible for nervousness. According to the World Health Organization (WHO), social networks protect mental health during the coronavirus epidemic, but mental health protection depends on personal behavior. Watching, reading, or hearing COVID-19 related news that makes people feel too nervous or upset should be reduced. Information can only be searched from reliable sources so that people will bring their plans into motion to defend themselves and members of their families. At particular times during the day, media can update their records once or twice. Anyone may be anxious about the unexpected and near-constant influx of news coverage about an epidemic. People should care about getting the facts by avoiding anecdotes and propaganda and assemble data from the World Health Organization’s website at regular intervals, and local health authority platforms also help you to differentiate facts from rumors [92]. Some news about spraying disinfectants from social media causes panic in general people [120], thus, it is essential to get actual information from authentic sources to manage the mental health-related problem.
In COVID-19 patients, social networking offers an interchange of encouragement and makes individuals feel less depressed because they can contact friends and family and feel community support. These will prevent one from boredom, loneliness, and monotonous situations. Social media gives information within a short time rather than moving outside, avoiding the speeding of SARS-CoV-2 infection. Viewers report to feel chills, excitement, and thrills; television is essential to compensate for the painful day-to-day routine during a pandemic situation. Positive newspaper coverage of COVID-19 related news help to prevent mental illness [121]. Ahmad (2020) suggests that authentic social media consumers on what constitutes good and reliable can play an essential role through younger since they use social media information to distribute it to their families and friends [118]. So in the case of the COVID-19 pandemic, educational facilities would be perfect locations to design classes and symposiums that will help students and teachers search, identify and analyze clinical knowledge that can mitigate mental health. To manage the mental health-related problem, special attention should be paid to depression and anxiety; various platforms like a hotline, online appointment, online course, and outpatient consultation can include mental health services by each country’s government.
Meditation
Meditation techniques are being used to treat and avoid a variety of mental disorders as it is a known and common method for controlling stress and mental health with well-being and change in both cognitive and memory functions, regulate social and emotional behavior and help to improve in various, cardiovascular, neurological, autoimmune pathologies [114, 115]. Meditation can be an alternative therapy and may become an adjunctive for treating and managing mental health patients infected with SARS-CoV-2. The effects of meditation are based on endocrine system regulation, including the renin-angiotensin-aldosterone system (RAAS), the hypothalamic-pituitary-adrenal, and the thyroid axis with energy homeostasis [123]. Besides, mindfulness meditation can increase anti-inflammatory glucocorticoid receptor activity and induce type I interferon signaling called transcription factor associated with SARS-CoV-2 treatment [124]. Meditative practices can regulate the immune system that can help to mitigate stress. Several studies reported that meditation decreased activity of pro-inflammatory cytokines including C-reactive protein (CRP) and interleukin ( IL-6, IL-12), nuclear factor kappa B (NF-kB), natural killer (NK), and production of NK and T cell cytokine with promoting anti-inflammatory molecules such as IL-10 activity [117 – 122]. Furthermore, yoga or therapies are directly linked with the expression of antimicrobial peptides, including β-defensin and HBD-2. These two mentioned antimicrobial peptides are usually expressed in the lungs’ epithelial cells associated with COVID-19 infections [123, 124]. The expression of the anti-apoptotic genes BCL-2, COX-2, and HSP-70, a stress response gene, increased dramatically and prevented stress-related apoptosis by meditation [133]. Meditation is related to epigenetic control, and pilot studies indicate that insight meditation training can reduce inflammation, cell ageing, and depression linked to the epigenetic pathways [134]. The practice of meditation triggers neurotransmitters that modulate psychological disorders such as anxiety. For instance, meditation increased GABA and serotonin levels, while decreased norepinephrine (NE) levels help to decrease anxiety levels [135]. A Comparative Study by Sharma et al. reported that meditation could regulate antioxidant enzymes like dismutase (SOD), catalase, and glutathione enzyme production those could alleviate oxidative stress-mediated psychosocial stress [128, 129]. The application of meditation apps to alleviate anxiety with simultaneously improving wellbeing at the time of COVID-19 pandemic can be an alternative way to manage mental health. A randomized, controlled trial was designed to make relationship between daily use of a mindfulness app on measures of participant anxiety and feeling of wellbeing as well as perception of the situations during the COVID-19 pandemic [138].
Meditation may potentially enhance melatonin activity, which has been tested for possible treatment against COVID-19 [95]. In a clinical trial, 60 patients with COVID-19 patients, melatonin recovered some significant clinical symptoms and oxygen saturation and improved serum inflammatory molecules [89]. Matiz et al. reported that a study in Italy among 66 patients, through mindfulness-based training might effectively mitigate the negative psychological impact of the COVID-19 outbreak and improve wellbeing in the most vulnerable individuals [139]. Behan (2020) reported that the introduction of mindfulness and meditation practice during the COVID-19 pandemic could complement treatment and provide support with suppressing anxiety for all [140]. A cross-sectional study was done by Jiménez (2020) with 412 participants and found that self-compassion was related to better cohabitation during confinement with improving mental health and COVID-19 epidemic [141]. According to a review on mindfulness meditation among 47 trials with 3515 participants based study, mindfulness meditation programs had moderate evidence of improved anxiety, depression, and pain [142]. In a Randomized Controlled Trial by Hoge et al. (2013), mindfulness-based stress reduction (MBSR) contributes to decreasing anxiety-like symptoms such as anxiety disorder (GAD) with improving stress reactivity [143].
CONCLUSIONS
The COVID-19 pandemic is widely regarded as one of the most severe threats to global health systems in the twenty-first century. The latest coronavirus has developed immense psychological challenges beyond the physical and geographical problem in different subpopulations around every country, especially industrialized countries. Several factors can be attributed to deal with the negative effect of mental health during the disease outbreak. This narrative research discovered that individuals’ characteristics might significantly mitigate psychological behavior, including depression, panic attack, stress, emotional disturbance and somatization, suicidal behavior, sleep disorders, anxiety, post-traumatic stress disorder (PTSD) symptoms, and many additional mental health issues. Physical activity and the maintenance of safe sleeping habits may be beneficial. These are considered mitigation techniques for average citizens forced to remain at home, both cost-effective and realistic.
To decrease quarantine-related situational stress, immuno-supportive nutrients play an essential function in improving the brain’s negative effect. Furthermore, during the time of the pandemic, motivation from a family member as well as others can improve confidence level and support to the management of the psychological problem, especially health workers. Social media can play another vital role in the teenager by publishing authentic news that will mitigate depression and anxiety in individuals. In COVID-19 patients, meditation works to mitigate psychological behavior by enhancing resilience and improving well-being during an emergency crisis. Overall, our study’s knowledge to be valuable, meaningful, and appropriate to cope with mental stress caused by SARS-CoV-2. We recommend all people follow the complete package of guidance, including exercise, diet, proper sleep, motivation, social media, and meditation, to manage mental health during this COVID-19 crisis.
ACKNOWLEDGEMENT
None.
AUTHOR CONTRIBUTIONS
MS, MAH, and MKH were involved in conception and design of the experiments. AH and MSH contributed to drafting the article. MNA and TBE contributed to revising it critically for important intellectual content. All authors made the final approval of the version to be published.
CONFLICTS OF INTEREST
There is no conflict of interest among the authors.
References
- [1]Liu YC, Kuo RL, Shih SR. COVID-19: The first documented coronavirus pandemic in history. Biomed J 2020;43:328–33.
- [2]Zheng J. SARS-coV-2: An emerging coronavirus that causes a global threat. Int J Biol Sci 2020;16:1678–85.
- [3]Sotgiu G, Dobler CC. Social stigma in the time of coronavirus disease 2019. Eur Respir J 2020;56.
- [4]Talevi D, Socci V, Carai M, Carnaghi G, Faleri S, Trebbi E, et al. Mental health outcomes of the covid-19 pandemic. Riv Psichiatr 2020;55:137–44.
- [5]Zhang Y, Zhang H, Ma X, Di Q. Mental health problems during the COVID-19 pandemics and the mitigation effects of exercise: A longitudinal study of college students in China. Int J Environ Res Public Health 2020;17.
- [6]Shultz JM, Cooper JL, Baingana F, Oquendo MA, Espinel Z, Althouse BM, et al. The Role of Fear-Related Behaviors in the 2013–2016 West Africa Ebola Virus Disease Outbreak. Curr Psychiatry Rep 2016;18:104.
- [7]De Brier N, Stroobants S, Vandekerckhove P, De Buck E. Factors affecting mental health of health care workers during coronavirus disease outbreaks (SARS, MERS & COVID-19): A rapid systematic review. PLoS One 2020;15:e0244052.
- [8]Pfefferbaum B, Schonfeld D, Flynn BW, Norwood AE, Dodgen D, Kaul RE, et al. The H1N1 crisis: A case study of the integration of mental and behavioral health in public health crises. Disaster Med Public Health Prep 2012;6:67–71.
- [9]Khan S, Siddique R, Xiaoyan W, Zhang R, Nabi G, Sohail Afzal M, et al. Mental health consequences of infections by coronaviruses including severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Brain Behav 2021;11:e01901.
- [10]Li S, Wang Y, Xue J, Zhao N, Zhu T. The impact of covid-19 epidemic declaration on psychological consequences: A study on active weibo users. Int J Environ Res Public Health 2020;17.
- [11]Frasquilho D, Matos MG, Salonna F, Guerreiro D, Storti CC, Gaspar T, et al. Mental health outcomes in times of economic recession: A systematic literature review Health behavior, health promotion and society. BMC Public Health 2016;16.
- [12]Shammi M, Bodrud-Doza M, Towfiqul Islam ARM, Rahman MM. COVID-19 pandemic, socioeconomic crisis and human stress in resource-limited settings: A case from Bangladesh. Heliyon 2020;6.
- [13]Zhai Y, Du X. Addressing collegiate mental health amid COVID-19 pandemic. Psychiatry Res 2020;288.
- [14]Magson NR, Freeman JYA, Rapee RM, Richardson CE, Oar EL, Fardouly J. Risk and Protective Factors for Prospective Changes in Adolescent Mental Health during the COVID-19 Pandemic. J Youth Adolesc 2021;50:44–57.
- [15]Neria Y, Sullivan GM. Understanding the mental health effects of indirect exposure to mass trauma through the media. JAMA – J Am Med Assoc 2011;306:1374–5.
- [16]Chew QH, Wei KC, Vasoo S, Chua HC, Sim K. Narrative synthesis of psychological and coping responses towards emerging infectious disease outbreaks in the general population: Practical considerations for the COVID-19 pandemic. Singapore Med J 2020;61:350–6.
- [17]Fardin MA. Covid-19 and anxiety: A review of psychological impacts of infectious disease outbreaks. Arch Clin Infect Dis 2020;15.
- [18]Goodwin GM. Depression and associated physical diseases and symptoms. Dialogues Clin Neurosci 2006;8:259–65.
- [19]Mamun MA, Griffiths MD. First COVID-19 suicide case in Bangladesh due to fear of COVID-19 and xenophobia: Possible suicide prevention strategies. Asian J Psychiatr 2020;51.
- [20]Gao J, Zheng P, Jia Y, Chen H, Mao Y, Chen S, et al. Mental health problems and social media exposure during COVID-19 outbreak. PLoS One 2020;15.
- [21]Seminog OO, Goldacre MJ. Risk of pneumonia and pneumococcal disease in people with severe mental illness: English record linkage studies. Thorax 2013;68:171–6.
- [22]Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav Immun 2020;88:901–7.
- [23]González-Sanguino C, Ausín B, Castellanos MÁ, Saiz J, López-Gómez A, Ugidos C, et al. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain Behav Immun 2020;87:172–6.
- [24]Wu C, Yang L, Li Y, Dong YAN, Yang B, Tucker LD, et al. Effects of Exercise Training on Anxious-Depressive-like Behavior in Alzheimer Rat. Med Sci Sports Exerc 2020;52:1456–69.
- [25]Stonerock GL, Hoffman BM, Smith PJ, Blumenthal JA. Exercise as Treatment for Anxiety: Systematic Review and Analysis. Ann Behav Med 2015;49:542–56.
- [26]Wegner M, Helmich I, Machado S, Nardi A, Arias-Carrion O, Budde H. Effects of Exercise on Anxiety and Depression Disorders: Review of Meta- Analyses and Neurobiological Mechanisms. CNS Neurol Disord – Drug Targets 2014;13:1002–14.
- [27]Harvey SB, Overland S, Hatch SL, Wessely S, Mykletun A, Hotopf M. Exercise and the prevention of depression: Results of the HUNT cohort study. Am J Psychiatry 2018;175:28–36.
- [28]Carek PJ, Laibstain SE, Carek SM. Exercise for the treatment of depression and anxiety. Int J Psychiatry Med 2011;41:15–28.
- [29]Jurak G, Morrison SA, Leskošek B, Kovač M, Hadžić V, Vodičar J, et al. Physical activity recommendations during the coronavirus disease-2019 virus outbreak. J Sport Heal Sci 2020;9:325–7.
- [30]Gleeson M. Immune function in sport and exercise. J Appl Physiol 2007;103:693–9.
- [31]Simpson RJ, Kunz H, Agha N, Graff R. Exercise and the Regulation of Immune Functions. Prog. Mol. Biol. Transl. Sci., vol. 135, 2015, p. 355–80.
- [32]Song M, Chan AT. The Potential Role of Exercise and Nutrition in Harnessing the Immune System to Improve Colorectal Cancer Survival. Gastroenterology 2018;155:596–600.
- [33]Sleiman SF, Henry J, Al-Haddad R, El Hayek L, Haidar EA, Stringer T, et al. Exercise promotes the expression of brain derived neurotrophic factor (BDNF) through the action of the ketone body β- hydroxybutyrate. Elife 2016;5.
- [34]Daniele TM da C, de Bruin PFC, Rios ERV, de Bruin VMS. Effects of exercise on depressive behavior and striatal levels of norepinephrine, serotonin and their metabolites in sleep-deprived mice. Behav Brain Res 2017;332:16–22.
- [35]Patki G, Li L, Allam F, Solanki N, Dao AT, Alkadhi K, et al. Moderate treadmill exercise rescues anxiety and depression-like behavior as well as memory impairment in a rat model of posttraumatic stress disorder. Physiol Behav 2014;130:47–53.
- [36]Passos GS, Poyares D, Santana MG, Teixeira AADS, Lira FS, Youngstedt SD, et al. Exercise improves immune function, antidepressive response, and sleep quality in patients with chronic primary insomnia. Biomed Res Int 2014;2014.
- [37]Woods JA, Vieira VJ, Keylock KT. Exercise, Inflammation, and Innate Immunity. Immunol Allergy Clin North Am 2009;29:381–93.
- [38]Anderson E, Shivakumar G. Effects of exercise and physical activity on anxiety. Front Psychiatry 2013;4.
- [39]Mogg K, Bradley BP. Anxiety and Threat-Related Attention: Cognitive-Motivational Framework and Treatment. Trends Cogn Sci 2018;22:225–40
- [40]Michopoulos V, Powers A, Gillespie CF, Ressler KJ, Jovanovic T. Inflammation in Fear-and Anxiety-Based Disorders: PTSD, GAD, and beyond. Neuropsychopharmacology 2017;42:254–70.
- [41]Adlard PA, Cotman CW. Voluntary exercise protects against stress-induced decreases in brain-derived neurotrophic factor protein expression. Neuroscience 2004;124:985–92.
- [42]Khawam E, Khouli H, Pozuelo L. Treating acute anxiety in patients with COVID-19: Posted april 26, 2020. Cleve Clin J Med 2020;87:1–4.
- [43]Liu PZ, Nusslock R. Exercise-mediated neurogenesis in the hippocampus via BDNF. Front Neurosci 2018;12.
- [44]Lopresti AL, Hood SD, Drummond PD. A review of lifestyle factors that contribute to important pathways associated with major depression: Diet, sleep and exercise. J Affect Disord 2013;148:12–27.
- [45]Abd El-Kader SM, Al-Jiffri OH. Exercise alleviates depression related systemic inflammation in chronic obstructive pulmonary disease patients. Afr Health Sci 2016;16:1078–88.
- [46]Heyn P, Abreu BC, Ottenbacher KJ. The effects of exercise training on elderly persons with cognitive impairment and dementia: A meta-analysis. Arch Phys Med Rehabil 2004;85:1694–704.
- [47]World Health Organization. WHO EMRO | Nutrition advice for adults during the COVID-19 outbreak | Nutrition-infocus | Nutrition. Nutr Advice Adults Dur COVID-19 Outbreak 2020. http://www.emro.who.int/nutrition/nutrition-infocus/nutrition-advice-for-adults-during-the-covid-19-outbreak.html (accessed January 16, 2021).
- [48]athyanarayana Rao T, Asha M, Ramesh B, Jagannatha Rao K. Understanding nutrition, depression and mental illnesses. Indian J Psychiatry 2008;50:77.
- [49]Nieman DC. Influence of carbohydrate on the immune response to intensive, prolonged exercise. Exerc Immunol Rev 1998:64–76.
- [50]Rodríguez-Valentín M, López S, Rivera M, Ríos-Olivares E, Cubano L, Boukli NM. Naturally derived anti-HIV polysaccharide peptide (PSP) triggers a toll-like receptor 4-dependent antiviral immune response. J Immunol Res 2018;2018.
- [51]Hou YC, Liou KT, Chern CM, Wang YH, Liao JF, Chang S, et al. Preventive effect of silymarin in cerebral ischemia-reperfusion-induced brain injury in rats possibly through impairing NF-κB and STAT-1 activation. Phytomedicine 2010;17:963–73.
- [52]Ciok J, Dolna A. Wȩglowodany a sprawność umysłowa – Znaczenie indeksu glikemicznego. Pol Merkur Lek 2006;20:367–70.
- [53]Owen L, Finnegan Y, Hu H, Scholey AB, Sünram-Lea SI. Glucose effects on long-term memory performance: Duration and domain specificity. Psychopharmacology (Berl) 2010;211:131–40.
- [54]Hoyland A, Dye L, Lawton CL. A systematic review of the effect of breakfast on the cognitive performance of children and adolescents. Nutr Res Rev 2009;22:220–43.
- [55]Benton D, Ruffin MP, Lassel T, Nabb S, Messaoudi M, Vinoy S, et al. The delivery rate of dietary carbohydrates affects cognitive performance in both rats and humans. Psychopharmacology (Berl) 2003;166:86–90.
- [56]Van De Rest O, Van Der Zwaluw NL, De Groot LCPGM. Literature review on the role of dietary protein and amino acids in cognitive functioning and cognitive decline. Amino Acids 2013;45:1035–45.
- [57]Khaliq S, Haider S, Ahmed SP, Perveen T, Haleem DJ. Relationship of brain tryptophan and serotonin in improving cognitive performance in rats. Pak J Pharm Sci 2006;19:11–5.
- [58]Wycherley TP, Moran LJ, Clifton PM, Noakes M, Brinkworth GD. Effects of energy-restricted high-protein, low-fat compared with standard-protein, low-fat diets: A meta-analysis of randomized controlled trials. Am J Clin Nutr 2012;96:1281–98.
- [59]Muscogiuri G, Barrea L, Savastano S, Colao A. Nutritional recommendations for CoVID-19 quarantine. Eur J Clin Nutr 2020;74:850–1.
- [60]Hunsche C, Hernandez O, Gheorghe A, Díaz LE, Marcos A, De la Fuente M. Immune dysfunction and increased oxidative stress state in diet-induced obese mice are reverted by nutritional supplementation with monounsaturated and n-3 polyunsaturated fatty acids. Eur J Nutr 2018;57:1123–35.
- [61]Laskin DL, Sunil VR, Gardner CR, Laskin JD. Macrophages and tissue injury: Agents of defense or destruction? Annu Rev Pharmacol Toxicol 2011;51:267–88.
- [62]Das UN. Response to: Bioactive Lipids and Coronavirus (COVID-19)-further Discussion. Arch Med Res 2020;51:445–9.
- [63]Das UN. Can Bioactive Lipids Inactivate Coronavirus (COVID-19)? Arch Med Res 2020;51:282–6.
- [64]Zhou P, Yang X Lou, Wang XG, Hu B, Zhang L, Zhang W, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 2020;579:270–3.
- [65]Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S, et al. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell 2020;181:271-280.e8.
- [66]Carr AC, Maggini S. Vitamin C and immune function. Nutrients 2017;9.
- [67]Farjana M, Moni A, Sohag AAM, Hasan A, Hannan MA, Hossain MG, et al. Repositioning vitamin c as a promising option to alleviate complications associated with COVID-19. Infect Chemother 2020.
- [68]McCartney DM, Byrne DG. Optimisation of vitamin d status for enhanced immuno-protection against covid-19. Ir Med J 2020;113.
- [69]Baksi SN, Hughes MJ. Chronic vitamin D deficiency in the weanling rat alters catecholamine metabolism in the cortex. Brain Res 1982;242:387–90.
- [70]Benton D, Haller J, Fordy J. Vitamin supplementation for 1 year improves mood. Neuropsychobiology 1995;32:98–105.
- [71]Bourre JM. Effects of nutrients (in food) on the structure and function of the nervous system: Update on dietary requirements for brain. Part 2: Macronutrients. J Nutr Heal Aging 2006;10:386–99.
- [72]Name JJ, Souza ACR, Vasconcelos AR, Prado PS, Pereira CPM. Zinc, Vitamin D and Vitamin C: Perspectives for COVID-19 With a Focus on Physical Tissue Barrier Integrity. Front Nutr 2020;7:295.
- [73]Wessels I, Maywald M, Rink L. Zinc as a gatekeeper of immune function. Nutrients 2017;9.
- [74]te Velthuis AJW, van den Worml SHE, Sims AC, Baric RS, Snijder EJ, van Hemert MJ. Zn2+ inhibits coronavirus and arterivirus RNA polymerase activity in vitro and zinc ionophores block the replication of these viruses in cell culture. PLoS Pathog 2010;6.
- [75]Golub MS, Keen CL, Gershwin ME, Hendrickx AG. Developmental zinc deficiency and behavior. J. Nutr., vol. 125, 1995.
- [76]Maggini S, Pierre A, Calder PC. Immune function and micronutrient requirements change over the life course. Nutrients 2018;10.
- [77]Alpert PT. The Role of Vitamins and Minerals on the Immune System. Home Heal Care Manag Pract 2017;29:199–202.
- [78]Saeed F, Nadeem M, Ahmed RS, Tahir Nadeem M, Arshad MS, Ullah A. Studying the impact of nutritional immunology underlying the modulation of immune responses by nutritional compounds – a review. Food Agric Immunol 2016;27:205–29.
- [79]Maggini S, Wintergerst ES, Beveridge S, Hornig DH. Selected vitamins and trace elements support immune function by strengthening epithelial barriers and cellular and humoral immune responses. Br. J. Nutr., vol. 98, 2007. https://doi.org/10.1017/S0007114507832971.
- [80]Sankar R, Rai B, Pulger T, Sankar G, Srinivasan T, Srinivasan L, et al. Intellectual and motor functions in school children from severely iodine deficienct region in Sikkim. Indian J Pediatr 1994;61:231–6.
- [81]Hossain KS, Hossain MG, Moni A, Rahman MM, Rahman UH, Alam M, et al. Prospects of honey in fighting against COVID-19: pharmacological insights and therapeutic promises. Heliyon 2020.
- [82]Zareie PP. Honey as an antiviral agent against respiratory syncytial virus 2011.
- [83]Abedi F, Ghasemi S, Farkhondeh T, Azimi-Nezhad M, Shakibaei M, Samarghandian S. Possible Potential Effects of Honey and Its Main Components Against Covid-19 Infection. Dose-Response 2021.
- [84]Islam MN, Hossain KS, Sarker PP, Ferdous J, Hannan MA, Rahman MM, et al. Revisiting pharmacological potentials of Nigella sativa seed: A promising option for COVID-19 prevention and cure. Phyther Res 2021.
- [85]Ulasli M, Gurses SA, Bayraktar R, Yumrutas O, Oztuzcu S, Igci M, et al. The effects of Nigella sativa (Ns), Anthemis hyalina (Ah) and Citrus sinensis (Cs) extracts on the replication of coronavirus and the expression of TRP genes family. Mol Biol Rep 2014.
- [86]Forouzanfar F, Fazly Bazzaz BS, Hosseinzadeh H. Black cumin (Nigella sativa) and its constituent (thymoquinone): A review on antimicrobial effects. Iran J Basic Med Sci 2014.
- [87]Koshak AE, Koshak EA, Mobeireek AF, Badawi MA, Wali SO, Malibary HM, et al. Nigella sativa supplementation to treat symptomatic mild COVID-19: A structured summary of a protocol for a randomised, controlled, clinical trial. Trials 2020;21:703.
- [88]Hassaniazad M, Inchehsablagh BR, Kamali H, Tousi A, Eftekhar E, Jaafari MR, et al. The clinical effect of Nano micelles containing curcumin as a therapeutic supplement in patients with COVID-19 and the immune responses balance changes following treatment: A structured summary of a study protocol for a randomised controlled trial. Trials 2020;21:1–3.
- [89]Ziaei A, Davoodian P, Dadvand H, Safa O, Hassanipour S, Omidi M, et al. Evaluation of the efficacy and safety of Melatonin in moderately ill patients with COVID-19: A structured summary of a study protocol for a randomized controlled trial. Trials 2020;21.
- [90]Bao Y, Sun Y, Meng S, Shi J, Lu L. 2019-nCoV epidemic: address mental health care to empower society. Lancet 2020;395:e37–8.
- [91]Franceschini C, Musetti A, Zenesini C, Palagini L, Scarpelli S, Quattropani MC, et al. Poor sleep quality and its consequences on mental health during the COVID-19 lockdown in Italy. Front Psychol 2020;11:1–15.
- [92]WHO/2019-nCoV/MentalHealth/2020.1. Mental Health and Psychosocial Considerations During COVID-19 Outbreak. World Heal Organ 2020;1:1–6.
- [93]Hannan M, Islam M, Uddin M. Self-confidence as an immune-modifying psychotherapeutic intervention for COVID-19 patients and understanding of its connection to CNS-endocrine-immune axis. J Adv Biotechnol Exp Ther 2020
- [94]Seithikurippu R AM. Melatonin, the Hormone of Darkness: From Sleep Promotion to Ebola Treatment. Brain Disord Ther 2015;04.
- [95]Zhang R, Wang X, Ni L, Di X, Ma B, Niu S, et al. COVID-19: Melatonin as a potential adjuvant treatment. Life Sci 2020;250.
- [96]Everson CA, Laatsch CD, Hogg N. Antioxidant defense responses to sleep loss and sleep recovery. Am J Physiol – Regul Integr Comp Physiol 2005;288.
- [97]Vaccaro A, Kaplan Dor Y, Nambara K, Pollina EA, Lin C, Greenberg ME, et al. Sleep Loss Can Cause Death through Accumulation of Reactive Oxygen Species in the Gut. Cell 2020;181:1307-1328.e15.
- [98]Mirmiran M, Scholtens J, Van de Poll NE, Uylings HBM, Van der Gugten J, Boer GJ. Effects of experimental suppression of active (REM) sleep during early development upon adult brain and behavior in the rat. Dev Brain Res 1983;7:277–86.
- [99]Frank MG, Heller HC. The ontogeny of mammalian sleep: A reappraisal of alternative hypotheses. J Sleep Res 2003;12:25–34.
- [100]Tononi G, Cirelli C. Sleep and the Price of Plasticity: From Synaptic and Cellular Homeostasis to Memory Consolidation and Integration. Neuron 2014;81:12–34.
- [101]Ragab D, Salah Eldin H, Taeimah M, Khattab R, Salem R. The COVID-19 Cytokine Storm; What We Know So Far. Front Immunol 2020;11.
- [102]Milrad SF, Hall DL, Jutagir DR, Lattie EG, Ironson GH, Wohlgemuth W, et al. Poor sleep quality is associated with greater circulating pro-inflammatory cytokines and severity and frequency of chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME) symptoms in women. J Neuroimmunol 2017;303:43–50.
- [103]Besedovsky L, Lange T, Haack M. The sleep-immune crosstalk in health and disease. Physiol Rev 2019;99:1325–80.
- [104]Miller GE, Cohen S, Pressman S, Barkin A, Rabin BS, Treanor JJ. Psychological Stress and Antibody Response to Influenza Vaccination: When Is the Critical Period for Stress, and How Does It Get Inside the Body? Psychosom Med 2004;66:215–23.
- [105]Lallukka T, Sivertsen B. Sleep improvement by internet-based cognitive behavioural therapy might help prevent mental health disorders. The Lancet Psychiatry 2017;4:734–5.
- [106]Teker AG. Sleep Quality and Anxiety Level in Employees. North Clin Istanbul 2017.
- [107]Shamsaei F, Daraei MM, Aahmadinia H, Khalili A, Seif M. The relationship between sleep habits and mental health in Iranian elementary school children. Sleep Sci 2019;12:94–9.
- [108]Ojio Y, Nishida A, Shimodera S, Togo F, Sasaki T. Sleep duration associated with the lowest risk of depression/anxiety in adolescents. Sleep 2016;39:1555–62.
- [109]Supartini A, Honda T, Basri NA, Haeuchi Y, Chen S, Ichimiya A, et al. The Impact of Sleep Timing, Sleep Duration, and Sleep Quality on Depressive Symptoms and Suicidal Ideation amongst Japanese Freshmen: The EQUSITE Study. Sleep Disord 2016;2016:1–10.
- [110]Morgan GA, Harmon RJ, Maslin-Cole CA. Mastery motivation: Definition and measurement. Early Educ Dev 1990;1:318–39.
- [111]Karatepe OM, Uludag O. Conflict, exhaustion, and motivation: A study of frontline employees in Northern Cyprus hotels. Int J Hosp Manag 2007;26:645–65.
- [112]Tsutsumi A, Nagami M, Morimoto K, Kawakami N. Motivation, overcommitment and psychological health at work: A path analytic approach. J UOEH 2008;30:279–92.
- [113]Wegge J, Van Dick R, Fisher G, Wecking C, Moltzen K. Work motivation, organisational identification, and well-being in call centre work. Work Stress 2006;20:60–83.
- [114]West R, Michie S, Rubin GJ, Amlôt R. Applying principles of behaviour change to reduce SARS-CoV-2 transmission. Nat Hum Behav 2020;4:451–9.
- [115]Firth J, Rosenbaum S, Stubbs B, Gorczynski P, Yung AR, Vancampfort D. Motivating factors and barriers towards exercise in severe mental illness: A systematic review and meta-analysis. Psychol Med 2016;46:2869–81.
- [116]Simpson EH, Balsam PD. The behavioral neuroscience of motivation: An overview of concepts, measures, and translational applications. Curr Top Behav Neurosci 2016;27:1–12.
- [117]Rodgers WM, Loitz CC. The role of motivation in behavior change: How do we encourage our clients to be active? vol. 13. 2009.
- [118]Ahmad AR, Murad HR. The impact of social media on panic during the COVID-19 pandemic in iraqi kurdistan: Online questionnaire study. J Med Internet Res 2020;22.
- [119]Ni MY, Yang L, Leung CMC, Li N, Yao XI, Wang Y, et al. Mental health, risk factors, and social media use during the COVID-19 epidemic and cordon sanitaire among the community and health professionals in wuhan, China: Cross-sectional survey. JMIR Ment Heal 2020;7.
- [120]Md Sohel -, Mahmod MR. Spraying Disinfectants to Combat SARS-CoV-2 Transmission: Is it Fruitless Rather Than Fruitful? Bangladesh J Infect Dis 2021;7:113–4.
- [121]Rhydderch D, Krooupa AM, Shefer G, Goulden R, Williams P, Thornicroft A, et al. Changes in newspaper coverage of mental illness from 2008 to 2014 in England. Acta Psychiatr Scand 2016;134:45–52.
- [122]Pascoe MC, Thompson DR, Ski CF. Meditation and Endocrine Health and Wellbeing. Trends Endocrinol Metab 2020;31:469–77.
- [123]Jindal V, Gupta S, Das R. Molecular mechanisms of meditation. Mol Neurobiol 2013;48:808–11.
- [124]Bower JE, Crosswell AD, Stanton AL, Crespi CM, Winston D, Arevalo J, et al. Mindfulness meditation for younger breast cancer survivors: A randomized controlled trial. Cancer 2015;121:1231–40.
- [125]Yoga, meditation counter gene expression changes that cause stress n.d. https://www.medicalnewstoday.com/articles/317946?fbclid=IwAR1HO1fbDxDDbpYzRmys0nIqX5IGtewxyXPkyGoYNrxF6NBv79vc3dpcIqE (accessed February 3, 2021).
- [126]Witek-Janusek L, Albuquerque K, Chroniak KR, Chroniak C, Durazo-Arvizu R, Mathews HL. Effect of mindfulness based stress reduction on immune function, quality of life and coping in women newly diagnosed with early stage breast cancer. Brain Behav Immun 2008;22:969–81.
- [127]Carlson LE, Speca M, Patel KD, Goodey E. Mindfulness-based stress reduction in relation to quality of life, mood, symptoms of stress, and immune parameters in breast and prostate cancer outpatients. Psychosom Med 2003;65:571–81.
- [128]Jang JH, Park HY, Lee US, Lee KJ, Kang DH. Effects of mind-body training on cytokines and their interactions with catecholamines. Psychiatry Investig 2017;14:483–90.
- [129]Cahn BR, Goodman MS, Peterson CT, Maturi R, Mills PJ. Yoga, meditation and mind-body health: Increased BDNF, cortisol awakening response, and altered inflammatory marker expression after a 3-month yoga and meditation retreat. Front Hum Neurosci 2017;11.
- [130]Jedel S, Hoffman A, Merriman P, Swanson B, Voigt R, Rajan KB, et al. A randomized controlled trial of mindfulness-based stress reduction to prevent flare-up in patients with inactive ulcerative colitis. Digestion 2014;89:142–55.
- [131]Eda N, Shimizu K, Suzuki S, Tanabe Y, Lee E, Akama T. Effects of yoga exercise on salivary beta-defensin 2. Eur J Appl Physiol 2013;113:2621–7.
- [132]Kim J, Yang YL, Jang SH, Jang YS. Human β-defensin 2 plays a regulatory role in innate antiviral immunity and is capable of potentiating the induction of antigen-specific immunity. Virol J 2018;15.
- [133]Saatcioglu F. Regulation of gene expression by yoga, meditation and related practices: A review of recent studies. Asian J Psychiatr 2013;6:74–7.
- [134]Kaliman P. Epigenetics and meditation. Curr Opin Psychol 2019;28:76–80.
- [135]Krishnakumar D, Hamblin MR, Lakshmanan S. Meditation and Yoga can Modulate Brain Mechanisms that affect Behavior and Anxiety- A Modern Scientific Perspective. Anc Sci 2015;2:13.
- [136]Donnelly GF. The relaxation response revisited. vol. 21. Morrow New York; 2007.
- [137]Sharma H, Sen S, Singh A, Bhardwaj NK, Kochupillai V, Singh N. Sudarshan Kriya practitioners exhibit better antioxidant status and lower blood lactate levels. Biol Psychol 2003;63:281–91.
- [138]O’Donnell KT, Dunbar M, Speelman DL. Effectiveness of using a meditation app in reducing anxiety and improving well-being during the COVID-19 pandemic: A structured summary of a study protocol for a randomized controlled trial. Trials 2020;21.
- [139]Matiz A, Fabbro F, Paschetto A, Cantone D, Paolone AR, Crescentini C. Positive impact of mindfulness meditation on mental health of female teachers during the COVID-19 outbreak in Italy. Int J Environ Res Public Health 2020;17:1–22.
- [140]Behan C. The benefits of meditation and mindfulness practices during times of crisis such as COVID-19. Ir J Psychol Med 2020;37:256–8.
- [141]Jiménez Ó, Sánchez-Sánchez LC, García-Montes JM. Psychological impact of COVID-19 confinement and its relationship with meditation. Int J Environ Res Public Health 2020;17:1–14.
- [142]Goyal M, Singh S, Sibinga EMS, Gould NF, Rowland-Seymour A, Sharma R, et al. Meditation programs for psychological stress and well-being: A systematic review and meta-analysis. JAMA Intern Med 2014;174:357–68.
- [143]Hoge EA, Bui E, Marques L, Metcalf CA, Morris LK, Robinaugh DJ, et al. Randomized controlled trial of mindfulness meditation for generalized anxiety disorder: Effects on anxiety and stress reactivity. J Clin Psychiatry 2013;74:786–92.