A study of arginase-1 activity and lipid profile in patients with myocardial infarction
Abstract
Myocardial necrosis caused by ischemia is called a myocardial infarction (MI). which interrupts coronary blood supply. When the oxygen supply to the heart is insufficient to meet metabolic demands, myocardial ischemia occurs. Atherosclerosis, which obstructs the coronary arteries, is the most common underlying cause of myocardial ischemia. The role of arginase-1 (ARG-1) and serum lipids in the pathogenesis of myocardial infarction is becoming clearer. This study aims to see if there is a link between ARG-1 activity and MI in the Iraqi population. Between the first of November 2021 and the first of February 2022, 90 people were separated into two groups: 45 patients with MI and 45 healthy controls. Human ARG-1 was measured in serum blood using the ELISA method. The serum lipid was measured using the spectrophotometry technique. The current investigation discovered a substantial (p=0.01) rise in ARG-1 concentration compared to control groups, as well as a significant difference in blood lipid content between patients and control groups (p<0.05). Finally, ARG-1 may have a role to play role in the pathogenesis of MI.
INTRODUCTION
Myocardial Infarction (MI) is the most common kind of vascular illness and the leading cause of death worldwide among all cardiovascular diseases (CVD) [1].The rupture, erosion, blockage, or blood clot formation in the coronary artery leads to stopped blood that reaches the heart causing a myocardial infarction disease. In addition, the heart cells may die as myocardial infarction causes permanent coronary artery blockage in about 30% of patients [2]. MI also refers to myocardial necrosis that occurs as a result of ischemia, which interrupts coronary blood flow. Ischemia causes necrosis in the sub-endocardial myocardium, which starts 15 to 20 minutes after the coronary artery is blocked [3]. A recent study suggests that arginase-1 (ARG1) has a role in the onset, progression, and consequences of MI [4].
Arginase- 1 (ARG-1) is one of the important enzymes in the urea cycle, which is universally called (EC: 3.5.3.1), and has a role in protein catabolism and ammonia breakdown [5, 6]. In addition, this enzyme was found in many cells and tissues, including phagocytic cells, endothelial cells, and smooth muscle, and it had a role in nitric oxidation and arginine metabolism in liver tissue [7]. Several studies reported that patients with myocardial infarction showed an increase in the concentration of arginase enzyme in the blood [8]. Where elevated ARG1 levels are inversely correlated with the left ventricular ejection fraction in patients, this enzyme could serve as a functional marker by which to detect an individual’s susceptibility to heart defects [9]. According to a 2007 study, blood total cholesterol is linked to cardiovascular disease in a favorable and substantial way (CVD). Cholesterol plays a critical role in the health of the human heart. High serum cholesterol levels are a major risk factor for human cardiovascular diseases like coronary artery disease and stroke. Plaque (a thick, hard deposit) can form in artery walls when too much cholesterol is in the blood [10].
Heart diseases cause many disorders in the body, including high levels of lipids in the body, especially triglycerides, so it can be considered a sign of dysfunction in the performance of the heart, in addition to the increase in the level of triglycerides and decrease in the levels of low-density lipoprotein (LDL) or vice versa causes atherosclerosis. It can increase the risk of stroke and heart attack as a result of the accumulation of fat in the walls of the arteries [11]. Another type of lipid called “good cholesterol” or high-density lipoprotein (HDL) is usually removed from body tissues and blood vessel walls by the liver. The amount of these lipids is inversely proportional to atherosclerosis, as the higher its concentration, the lower the incidence of disease. HDL transports cholesterol from other regions of the body to the liver, where it is excreted. As a result, HDL helps to prevent cholesterol from forming in the arteries’ walls [12].
LDL carries the majority of cholesterol in the blood, and LDL cholesterol is the primary cause of artery damage and blockage. As a result, the higher the level of LDL in human blood, the greater the risk of heart disease [13]. The liver is where very-low-density lipoprotein is made. Their diameter varies from 40 to 200 nm, depending on the quantity of their core lipid, particularly TG. TG and sterols are found in the liver (mostly CE). It also has other functions, including transporting triglycerides and fatty acids from the liver to the peripheral tissues [13]. VLDL remnants are a kind of VLDL that, like LDL, promotes atherosclerosis. VLDL remnants are made up of partially degraded VLDL and are high in cholesterol ester [14].
MATERIALS AND METHODS
Sample collection
This study design was a case-control study and was made in the clinical biochemistry laboratories of the College of the Medicine / University of Babylon. A total of 90 people took part in this prospective case-control study, 45 of whom had a myocardial infarction (45 patients) and 45 of whom appeared to be in good health. All the samples were obtained between November 1, 2021, and February 25, 2022. Marjan Teaching Hospital/ Shaheed Al-Mehrab Center in Hilla, Babylon Province, Iraq was used to collect samples.
Inclusion and exclusion criteria
Inclusion Criteria were the patients with Myocardial infarction. We have excluded the patients with renal disease, diabetic ketoacidosis (DKA), cardiogenic shock liver disease
Ethical statement
Written permissions were taken by volunteers before taking samples for research and the procedures for this research were carried out under the ethical approval numbered (DSM/HO-15314) for scientific research from the ethics committees of the Ministry of Higher Education and Scientific Research and the Iraqi Ministry of Health.
Biochemical analysis
The biochemical tests was making on the Myocardial infarction patients ranged in age from 42 to 73 years old, including the body mass index (BMI) equation test was used to show the ratio of weight to height in the body, which is often used by nutritionists to determine the weight as healthy or unhealthy [15], so the BMI (kg/m2 ) = weight (kg) / height (m2 ), and determination of Serum Arginase-1 in the patient and control groups by using ELISA assay from Bioassay (China) according to the manufacturer’s instructions, The plate has been pre-coated with Human ARG1 antibody. ARG1 present in the sample is added and binds to antibodies coated on the wells. Then biotinylated Human ARG1 antibody is added and binds to ARG1 in the sample. Then Streptavidin HRP is added and binds to the Biotinylated ARG1 antibody. After incubation unbound Streptavidin-HRP is washed away during a washing step. The substrate solution is then added, and color develops in proportion to the amount of Human ARG1. The reaction is terminated by the addition of acidic stop solution and absorbance is measured at 450 nm [16].
Determination of serum lipids
The concentrations of total cholesterol (TC), TG, HDL-C, LDL-C, and VLDL-C were determined using a spectrophotometric technique. Total cholesterol, Triglyceride, HDL-C kits Biolabo SA (France).
Determination of serum total cholesterol
Cholesterol concentration was determined enzymatically according to the method described by Allain C. et al. [17]. as shown in the following reactions
Determination of serum HDL-C
Chylomicron, LDL, and VLDL were precipitated by phosphotungstic acid and magnesium chloride. HDL-cholesterol obtained in the supernatant after centrifugation is then measured with TC reagent [18]
Determination of serum triglyceride (TG)
Triglyceride concentration was determined by an enzymatic procedure corresponding to the method expressed by Fossati P. and the principal method associated with the Trinder reaction, as shown in the following reactions [19]
The absorbance of the colored complex (quinonimine), at 500nm is proportional to the amount of triglycerides in the specimen.
Determination of serum VLDL-C
The concentration of VLDL-C was determined by dividing the triglyceride value, by 5 VLDL-cholesterol ((mg)⁄(dl)) = TG/5.
Determination of serum LDL-C
Concentration of LDL was calculated by using Fried Ewald equation. LDL-cholesterol (mg/dL) = Total-cholesterol − HDL-cholesterol – TG/ 5 [20].
Statistical analysis
The data were statistically analyzed using SPSS version 26, where the variables, percentages, variances, and mean of differences were found depending on the probability at p > 0.05 [16].
RESULTS
Demographic characteristics of the subject of study
Table 1 showed the mean age between myocardial infarction patients and the control group, where the percentage of infection of age ≥ 55 years shows at (71.2 %), while the patients with age ≤ 55 years show (28.8 %).
Table 1. The association between myocardial infarction patients and the control group according to age.
Determination of the body mass index in serum of MI patients
Table 2 showed the association between MI patients and the control group according to body mass index, where the mean of patients at 30.1 ± 3.74. the percentage of normal people group shows at (13.3 %), while in overweight group shows at (49%), in addition, the obese group shows at (37.7%).
Table 2. The association between patients and the control group according to body mass index.
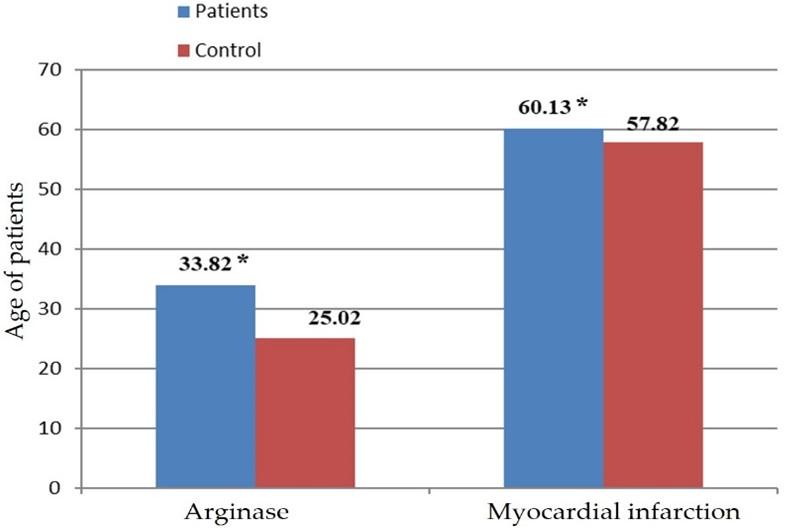
Determination of the arginase enzyme 1 in serum of MI patients
Figure 1 showed the mean correlation between the MI patients and arginase 1 activity, where the mean of patients shows at (33.5 ± 11.08), while the mean in the control group was (24.9 ± 6.56).
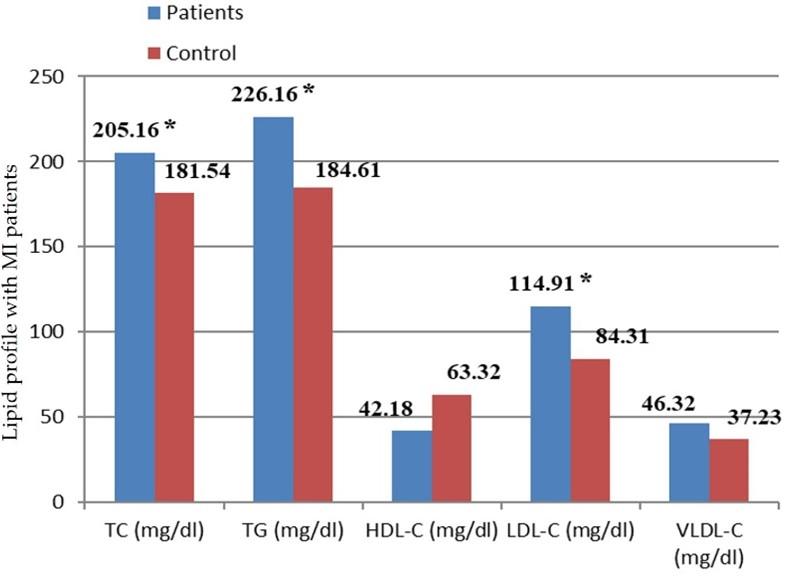
Determination of the lipid profile in serum of MI patients
Figure 2 showed the mean correlation between MI patients and lipid profile groups, where the mean of TC shows significant differences at (205.1 ± 53.64), TG show at (226.1 ± 68.03), HDL-C shows at (42.4 ± 9.28), LDL-C shows at (114.9 ± 39.5), and VLDL-C shows at (46.5± 13.6).
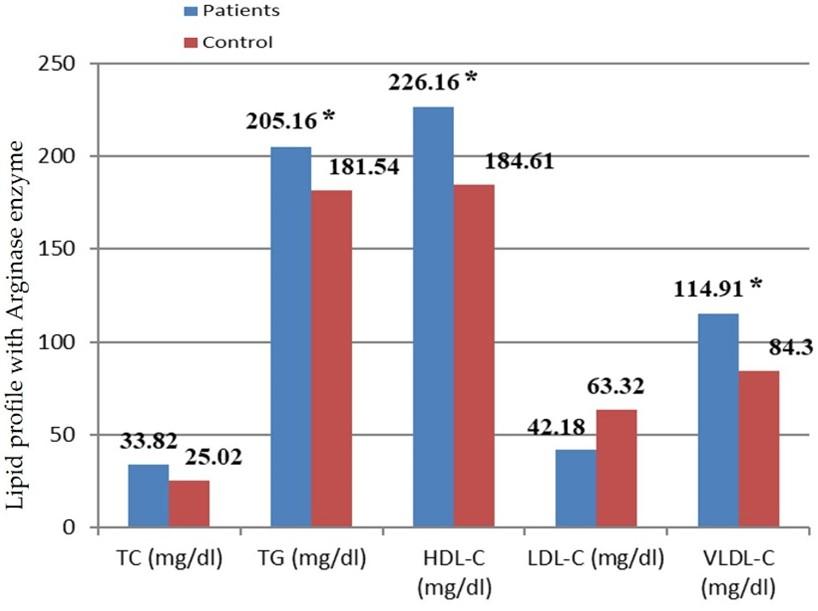
Figure 3 showed the mean correlation between arginase 1 activity and lipid profile groups, where the mean of TC shows significant differences at (205.16 ± 53.64), TG show at (226.16 ± 74.12), HDL-C shows at (42.18 ± 9.48), LDL-C shows at (114.91 ± 53.66), and VLDL-C shows at (46.32 ± 16.34).
DISCUSSION
In this study, it was found that most patients with MI fall within the age group of more than 55 years. These results are supported by research from around the world. Also, this study agrees with another which states that MI may occur at any age, but it occurs mainly in the age between 55-85 years old [17]. Many diseases are associated with age, including coronary atherosclerosis (CAD) and cardiovascular disease (CVD), where these diseases increase by 50% in people over the age of 60 years, so the highest incidence of coronary artery disease is in older patients age, which is often accompanied by an increase in morbidity and mortality rates [18].
The results that we obtained in Table 2 indicated that myocardial infarction disease was more incidence in obese /overweight people in contrast to the control group, this was consistent with the Yusuf et al [19] who found that the percentage of myocardial infraction was more in obese or overweight people compared to others. In addition, Sandfort et al [20] mentioned that there are many diseases whose morbidity increases with the increase in obesity, including diabetes mellitus, high blood pressure, and cardiovascular diseases, in addition to myocardial infarction, which may increase the death rate in these people.
In the current study, the percentage of arginase 1 enzyme was high in patients with myocardial infarction. These results were consistent with the study made by Shah et al [21] which indicated that there is a strong correlation between myocardial infarction and arginase 1, and the percentage of this enzyme increases with increased disease severity, which reached high rates compared to healthy controls. In addition, there is a statistically significant correlation between the ratio of arginase-1 enzyme and myocardial infarction patients, and it may be related to the development of symptoms of the disease and an increase in its severity [22–24].
Patients with atherosclerosis and during myocardial ischemia-reperfusion suffer from an increase in the activity and percentage of the enzyme arginase in the blood [25]. In addition, the study conducted by Molek et al. on patients with myocardial infarction indicated an increase in arginase that was due to the production of metabolism of eNOS to arginase 1, as well as an increase in the proportion of amino acids in plasma [26]. The experiments also showed the upregulation of the enzyme arginase 1 and its reperfusion after ischemia located at endothelial cells, smooth muscle cells, and cardiomyocytes [27]. Nitric Oxide (NO) has an important role in regulating cardiovascular homeostasis through its vasodilating, anti-inflammatory, and anti-thrombotic effects, and is an important protective factor against myocardial infarction and atherosclerosis [28, 29]. Atherosclerotic diseases and myocardial infarction lead to a dysfunction in the lining of blood vessels which causes an increase in competition of arginase 1 with nitric oxide synthase (NOS) for the common substrate – L-arginine due to an increase in its concentration and inhibits the biosynthesis of nitric oxide (NO) [30]. Therefore, an increase in arginase-1 activity leads to a decrease in the bioavailability of nitrogen oxide and an increase in susceptibility to ischemia and reperfusion infection, and these events lead to dysfunction and plaque formation in the vascular endothelium [31].
Lipid profile plays a pivotal role in the development of CVD [32]. The current study results were in agreement with a previous study done in Turkey, by Dun et al.,2019 that showed a statistically significant relationship between high TC levels and myocardial infarction incidence with a p-value (<0.05). They reported that increased TC in patients with MI than in the control group [32].
The increase in the concentration of cholesterol leads to the formation of some blood clots within the arteries, which can be carried by the blood to different parts and organs of the body. In addition, atherosclerosis leads to the narrowing of the walls of the blood vessels, which slows the movement of blood, and with the presence of blood clots, a myocardial infarction occurs [33], this was consistent with our study that shows increasing of cholesterol in the myocardial infarction patients. The researcher Folsom et al [34] mention that the incidence of myocardial infarction increases with increasing levels of both TG and LDL-C, in addition, triglycerides are considered one of the most prevalent types of lipids in the body, which is the result of increased body lipids and an increase in metabolic disturbances related to the abnormal concentration of TGs in the blood [35], which may increase the risk of developing myocardial infarction, as shown in Table 4 .
Results of the present study also agreed with a study by Park et al., [36] which showed a statistically significant relation between HDL-C levels and myocardial infraction with a p-value (<0.05) and mentioned that an increase in the ratio of HDL-C decreases the risk of cardiovascular disease, while a decrease in its ratio increases the risk of recurrent myocardial infarction and cardiovascular death [35, 37]. Another study by Michael V. Holmes, Iona Y. Millwood et al.,2018 in China showed a statistically significant relationship between high VLDL-C levels and myocardial infarction incidence with a p-value (<0.05) [6].
CONCLUSIONS
Myocardial Infarction seems to link with age and males are more susceptible than females. The high levels of ARGI in the patients compared to control may give an impression it may play a role in the pathogenesis of MI. High total cholesterol, triglycerides, VLDL-cholesterol, LDL-cholesterol, and low HDL-cholesterol concentrations are important risk factors in the development of coronary artery disease, so a complete lipid profile is always advisable.
ACKNOWLEDGEMENT
The authors would like to thank Dr. Yasir Haider Al-Mawlah and Dr. Ameer Mezher Hadi (DNA Research Center, University of Babylon. Pune for their kind support with all laboratory equipment and provide the suitable facilities, also for drafting the manuscript to make this work done.
AUTHOR CONTRIBUTIONS
Conception and design of the study: Ali A. Al-Anbari. Drafting the manuscript: Abdulsamie H. Alta’ee. Analysis and/or interpretation of data: Shokry F. Al-Saad.
CONFLICTS OF INTEREST
There is no conflict of interest among the authors.
References
- [1]M Sameen A, Qais Al-Ani M. Study of some physiological and biochemical aspects in the serum of myocardial infarction patients. Kirkuk University Journal-Scientific Studies 2011; 6: 63–72. DOI: 10.13140/RG.2.2.15106.84164
- [2]Walker BR, Colledge NR. Davidson’s principles and practice of medicine e-book. Elsevier Health Sciences, 2013.
- [3]Isaksson R-M. Symptoms, prehospital delay and long-term survival in men vs. women with myocardial infarction: a combined register and qualitative study. 2011; (Doctoral dissertation, Umeå universitet).
- [4]Tengbom J, Cederstrom S, Verouhis D, et al. P6599Upregulation of protein and gene expression of arginase-1 in patients with ST elevation myocardial infarction. European Heart Journal. 2019; 40: ehz746-1187.
- [5]Lee WY, Suh JY, Rhee EJ, et al. Plasma CRP, apolipoprotein A-1, apolipoprotein B and Lp(a) levels according to thyroid function status. Archives of Medical Research. 2004; 35(6): 540-545. DOI: 10.1016/j.arcmed.2004.08.003
- [6]Holmes M v., Millwood IY, Kartsonaki C, et al. Lipids, lipoproteins, and metabolites and risk of myocardial infarction and stroke. J Am Coll Cardiol. 2017; 71(6): 620-632. DOI: 10.1016/j.jacc.2017.12.006.
- [7]Kim PS, Iyer RK, Lu K v., et al. Expression of the liver form of arginase in erythrocytes. Molecular Genetics and Metabolism. 2002; 76(2): 100-110. DOI: 10.1016/S1096-7192(02)00034-3.
- [8]Teupser D, Burkhardt R, Wilfert W, et al. Identification of macrophage arginase I as a new candidate gene of atherosclerosis resistance. Arteriosclerosis, Thrombosis, and Vascular Biology. 2006; 26(2): 365-371. DOI: 10.1161/01.ATV.0000195791.83380.4c.
- [9]Gonon AT, Jung C, Katz A, et al. Local arginase inhibition during early reperfusion mediates cardioprotection via increased nitric oxide production. PLoS ONE. 2012; 7. DOI: 10.1371/journal.pone.0042038.
- [10]Bekpinar S, Gurdol F, Unlucerci Y, et al. Serum levels of arginase I are associated with left ventricular function after myocardial infarction. Clinical Biochemistry. 2011; 44(13): 1090-1093. DOI: 10.1016/j.clinbiochem.2011.06.003.
- [11]Patil V, Källqvist T, Olsen E, et al. Fatty acid composition of 12 microalgae for possible use in aquaculture feed. Aquaculture International. 2007; 15(1): 1-9. DOI: 10.1007/s10499-006-9060-3.
- [12]Bandeali S, Farmer J. High-density lipoprotein and atherosclerosis: The role of antioxidant activity. Current Atherosclerosis Reports. 2012; 14(2): 101-107. DOI: 10.1007/s11883-012-0235-2.
- [13]Segrest JP, Jones MK, de Loof H, et al. Structure of apolipoprotein B-100 in low density lipoproteins. Journal of Lipid Research. 2001; 42(9): 1346-1367. DOI: 10.1016/s0022-2275(20)30267-4.
- [14]Linton MF, Yancey PG, Davies SS, et al. The role of lipids and lipoproteins in atherosclerosis. Science (1979). 1950; 111(2877): 166-186.
- [15]Wahhab DN, Alta’ee AH, Hindawi AHAL. Assessment of circulating estrogen and osteoprotegerin levels in osteoporosis post-menopausal women in Babylon province. Biochem Cell Arch. 2020; 20(2): 4793-4796. DOI: 10.1210/jc.2002-020396
- [16]Green, S. B., Salkind, N. J., & Green, S. B. Using SPSS for windows and macintosh. Analyzing and understanding data. 2005.
- [17]Kim DH, Nah HW, Park HS, et al. Impact of prehospital intervention on delay time to thrombolytic therapy in a stroke center with a systemized stroke code program. Journal of Stroke and Cerebrovascular Diseases. 2016; 25(7): 1665-1670. DOI: 10.1016/j.jstrokecerebrovasdis.2016.02.011.
- [18]Wahhab DN, Alta’ee AH, al Hindawi AH. Assessment of circulating estrogen and osteoprotegerin levels in osteoporosis post-menopausal women in Babylon province. Biochem. Cell. Arch. 2020; 20(2): 4793-4796.
- [19]Yusuf S, Hawken S, Ôunpuu S, et al. Obesity and the risk of myocardial infarction in 27 000 participants from 52 countries: A case-control study. The Lancet. 2005; 366(9497): 1640-1649. DOI: 10.1016/S0140-6736(05)67663-5.
- [20]Sandfort V, Lai S, Ahlman MA, et al. Obesity is associated with progression of atherosclerosis during statin treatment. J Am Heart Assoc. 2016; 5(7): e003621. DOI: 10.1161/JAHA.116.003621.
- [21]Hussain Shah SR, Almugadam BS, Hussain A, et al. Epidemiology and risk factors of Helicobacter pylori infection in Timergara city of Pakistan: A cross-sectional study. Clinical Epidemiology and Global Health. 2021; 12: 100909. DOI: 10.1016/j.cegh.2021.100909.
- [22]North BJ, Sinclair DA. The intersection between aging and cardiovascular disease. Circulation Research. 2012; 110(8): 1097-1108. DOI: 10.1161/CIRCRESAHA.111.246876.
- [23]Tsai YY, Rainey WE, Johnson MH, et al. VLDL-activated cell signaling pathways that stimulate adrenal cell aldosterone production. Molecular and Cellular Endocrinology. 2016; 433: 138-146. DOI: 10.1016/j.mce.2016.05.018.
- [24]Menotti A, Scanga M, Morisi G. Serum triglycerides in the prediction of coronary artery disease (an Italian experience). The American Journal of Cardiology. 1994; 73(1): 29-32. DOI: 10.1016/0002-9149(94)90722-6.
- [25]Pernow J, Jung C. Arginase as a potential target in the treatment of cardiovascular disease: Reversal of arginine steal? Cardiovascular Research. 2013; 98(3): 334-343. DOI: 10.1093/cvr/cvt036.
- [26]Molek P, Zmudzki P, Wlodarczyk A, et al. The shifted balance of arginine metabolites in acute myocardial infarction patients and its clinical relevance. Scientific Reports. 2021; 11(1): 1-13. DOI: 10.1038/s41598-020-80230-3.
- [27]Hein TW, Zhang C, Wang W, et al. Ischemia‐reperfusion selectively impairs nitric oxide‐ mediated dilation in coronary arterioles: counteracting role of arginase. The FASEB Journal. 2003; 17(1)5: 2328-2330. DOI: 10.1096/fj.03-0115fje.
- [28]Durante W, Johnson FK, Johnson RA. Arginase: A critical regulator of nitric oxide synthesis and vascular function. Clinical and Experimental Pharmacology and Physiology. 2007; 34(9): 906. DOI: 10.1111/j.1440-1681.2007.04638.x.
- [29]Yasir Al-Mawlah, Alaa H, Aljelawi SO. Antibacterial activity of three plant extracts against multidrug resistance Pseudomonas Aeruginosa. Asian Journal of Pharmaceutical and Clinical Research. 2017; 10(12): 193-197. DOI: https://doi.org/10.22159/ajpcr.2017.v10i12.21071.
- [30]Santhanam L, Lim HK, Lim HK, et al. Inducible NO synthase-dependent S-nitrosylation and activation of arginase1 contribute to age-related endothelial dysfunction. Circulation Research. 2007; 101(7): 692-702. DOI: 10.1161/CIRCRESAHA.107.157727.
- [31]Romero MJ, Platt DH, Tawfik HE, et al. Diabetes-induced coronary vascular dysfunction involves increased arginase activity. Circulation Research. 2008; 102(1): 95-102. DOI: 10.1161/CIRCRESAHA.107.155028.
- [32]Dun Y, Thomas RJ, Medina-Inojosa JR, et al. High-intensity interval training in cardiac rehabilitation: impact on fat mass in patients with myocardial infarction. Mayo Clinic Proceedings. 2019; p: 1718-1730. DOI: 10.1016/j.mayocp.2019.04.033.
- [33]Lin HJ, Loh CH, Liao MT, et al. Attenuation of hypertriglyceridemia-induced pressor effect in rats with fructose-induced insulin resistance. Chinese Journal of Physiology. 2007; 50: 16-21. DOI: 10.1016/j.amjhyper.2004.04.006.
- [34]Folsom AR, Gottesman RF, Appiah D, et al. Plasma d-dimer and incident ischemic stroke and coronary heart disease: The atherosclerosis risk in communities study. Stroke. 2016; 47(1): 18-23. DOI: 10.1161/STROKEAHA.115.011035.
- [35]Duran EK, Aday AW, Cook NR, et al. Triglyceride-rich lipoprotein cholesterol, small dense LDL cholesterol, and incident cardiovascular disease. J Am Coll Cardiol. 2020; 75(17): 2122-2135. DOI: 10.1016/j.jacc.2020.02.059.
- [36]Park JS, Cha KS, Lee HW, et al. Predictive and protective role of high-density lipoprotein cholesterol in acute myocardial infarction. Cardiology Journal. 2019; 26(2): 176-185. DOI: 10.5603/CJ.a2018.0020.
- [37]Pellegrino D. Antioxidants and cardiovascular risk factors. Diseases. 2016; 4(1): 11. DOI: 10.3390/diseases4010011.