Antibiotic resistance pattern in the bacterial strains of urinary tract infection in Tangail city, Bangladesh
Abstract
Antimicrobial resistance has become an alarming issue all over the world. Moreover, in the developing countries as well as in Bangladesh facing this badly due to lack of study. Antibiotic resistance is prevalent among the bacterial pathogens causing urinary tract infections. Urinary tract infections affect >30% of people around the world. Worldwide, about 150 million people experience urinary tract infections each year. Antimicrobial treatment is often prescribed ‘empirically’ without antibiotic susceptibility testing to treat urinary tract infections (UTIs). The prevalence of antibiotic resistance is worsening, probably because of the increasing number of multidrug-resistant bacterial strains and the indiscriminate use of broad-spectrum antibiotics and empirical treatment. This study aims to determine the frequency and antibiotic resistance pattern of bacteria from suspected UTIs in Bangladeshi patients. In our study, about 200 samples of positive UTIs patients were analyzed with several parameters to see the antibiotic resistance rate. After examining the patient’s sample of UTIs antibiotic resistance rate is alarming and the most causative bacteria is Escherichia coli which is about 61.8%. Among the 200-urine sample suspected UTI patients 66% and 30% are female and male, respectively. Empirical therapy should be guided to control the antibiotic resistance. Especially, developing country should accept the challenge with proper infrastructure to get the surveillance of resistance, as resistance varies from region to region. Appropriate antibiotics should be focused for the rational use of antibiotics to prevent antibiotics resistance through common infections.
INTRODUCTION
The prevalence of antimicrobial resistance among microorganism that causes urinary tract infections (UTIs) is increasing worldwide including Bangladesh. UTIs narrate the presence of microbial pathogens within urinary tract [1]. UTIs can complicate any part of the urinary system including kidneys, bladder, ureters, and urethra. UTIs are commonly curable with broad-spectrum antibiotics. Most of the time antibiotics are prescribed without performing urine culture and sensitivity test. This inexact usage of antibiotics consequently has developed antibiotic resistance in bacteria. European survey of antibiotic consumption reported that multidrug resistant bacterial strains were liable for mortality rate about 25000 Europeans each year due to complications of UTIs [2]. This represents the scenario of UTIs worldwide why it is an urge to make termination of the use of inappropriate antibiotics, short or prolonged doses of antibiotics, self-medication just to inhibit the development of antibiotic resistance. Regional surveillance also should be guided to find susceptibility of microorganism in specific region [3]. Worldwide, about 150 million people experience urinary tract infections each year; resulting in 6 billion dollars in health care expenditure [4]. UTIs are responsible for affecting about 2 billion health care providers each year in the US [5]. Among the population about 60% of women and 12% of men will have at least one UTI during their lifetime [6]. UTIs are more frequent infection, accounting for nearly 25% of all infections (reference). Among all of the women in a population of a country about half of them will experience UTI during their lifetime. Nearly all UTIs (80%) are caused by uropathogenic E. coli (UPEC). Generally, bacteria enter into urinary tract system through urethra from skin or rectum, rarely through bloodstream. UTI is not sexually transmitted disease; even the infection is not itself contagious [7]. Bacteria which are present in person’s gut can relocate and grow in urinary tract resulting in UTIs. UTIs are fallen out more likely to female than male; it is about 3 times more female cases (6.6%) than male (1.8%) [1]. Hence female have shorter length of urethra than male, adding a reason to get UTI. The overall prevalence of UTI is approximately 7% in febrile infants and young children, pregnant women affecting as many as 8%, 20% women above 80 years, older ones are at risk of getting UTI randomly but varies by age, sex, and circumcision status [8-10]. UTIs are a severe public health problem which is caused by several pathogen including Escherichia coli, Klebsiella pneumoniae, Enterococcus faecalis, Staphylococcus saprophylicus, Proteus minabilis, and Pseudomans aeroginosa. UTIs are caused by both Gram-positive as well as Gram-negative bacteria. But most of the UTIs are occur by Gram-negative bacteria [11]. UTIs are differentiated in accordance with the site of infection developed by pathogen. They are-Pyelonephritis (kidneys), Cystitis (bladder), Bacteriuria (urine). According to the severity of complications, UTIs are clinically classified as complicated or uncomplicated. Uncomplicated UTI indicates that person have no structural or neurological abnormalities in urinary tract. Cystitis and Pyelonephritis are classified under uncomplicated UTIs. And complicated UTI indicates that patient have abnormal urinary tract and more susceptible to infection [12]. Broadly, antibiotics are empirically used to treat bacterial infections as well as UTIs without susceptibility tests leading to development of antibiotic resistance. Nowadays, development of antibiotic resistance is found as a global burden; expanded with alarming rate. Antibiotics resistance is the ability of bacteria to survive and grow on exposure to the antibiotics that were design to kill them or stop their growth [13]. Inexact dosage and empirical use of antibiotics, poor quality control of antibiotics, and poor surveillance of resistance development are denoted as the reason of antibiotic resistance [14]. Antibiotics resistance bacteria have no problem to grow, multiply and that is why causes infection easily within the host even after antibiotics exposed. This leads to serious problem and no longer be used antibiotics to treat successfully certain infection [15]. In developing country, antibiotic resistance spread more rapidly and become a matter of concern. In addition, its major contributors are developing countries like Bangladesh because of poor health care standard, the misuse and overuse of antibiotics. According to the WHO (2014) report on global surveillance of antimicrobial resistance and the report makes a clear case that resistance to common bacteria has reached alarming levels in many parts of the world and that in some settings [16]. Bangladesh, a developing country of Southeast Asia with high degree antibiotics resistance that passes a regional and global threat. The aim of this study was to analyze which type of bacteria was causing UTIs and the antibiotic resistance pattern among the people visiting a diagnostic centre at Tangail district to facilitate better treatment and management of UTIs.
MATERIALS AND METHODS
Study area
In our study, UTI patient samples were collected from Medinova Medical Services Limited hospital in the Tangail district, Bangladesh. Every sample was replicates for 3 times.
Study design
This is a cross-sectional prospective study, which was started from February 2021 to May 2021. Only UTI positive patients were selected and patient of Tangail district attending treatment in Medinova medical services limited were included in this study, sample number was about 200. The study was also approved by the ethical review committee of the Department of Biochemistry and Molecular Biology, Mawlana Bhashani Science and Technology University, Santosh, Tangail-1902, Bangladesh, with the certificate number MBSTU/BMB/TEST/2020/10(2).
Collection of urine sample for culture
A “clean catch” midstream urine sample was collected from the positive patient into the sterile leak proof bottles. First, patient needs to cleanse the urethral area to keep away contamination of the sample. In case of urinary catheter patient, urine samples were collected by using a fresh urinary catheter into a sterile sample tube.
Isolation and identification of uropathogens
To perform the isolation and identification of uropathogens each uniformly mixed raw midstream urine samples were culture into the MacConkey Agar (oxoid) and Sheep Blood Agar (Oxoid, Basingstoke, Hampshire,UK) media by using a standard calibrated loop (0.01ml). Plates were incubated at 37°C for 24hrs. Presence of 100,000 colony forming units (CFU) per milliliter in the culture was taken appropriate midstream urine sample and marked as positive urinary tract infection [17]. After incubation bacteria cultured on Muller Hinton broth (Becton, Dickinson and Company, USA), then bacteria were performed gram staining to determine gram positive or negative [18]. Performed microscopic analysis of bacteria for characterization on the basis of morphology [19]. And also performed appropriate biochemical test for proper identification [20].
Determination of antibiotic susceptibility
Identified bacteria was cultured in Muller Hinton agar for antibiotic susceptibility test by the Kirby-Bauer disk diffusion method based on clinical and laboratory standard institute 2012 [21]. Through analysis of zone of inhibition, it was determined that either antibiotic was resistant or sensitivity.
Statistical analysis
The data analysis is done by IBM SPSS Statistics version 24 (SPSS Inc., Chicago, IL, USA). Frequency distribution, Cross-tabulation, Chisquare test, Fisher exact test, Pie chart and Bar chart were applied for the statistical estimation of the variables. The study was preceded through the frequency and percentage analysis of attributes by SPSS. The graph is designed with Python programming language by python matplotilb libraries.
RESULTS
Percentage of isolated organisms
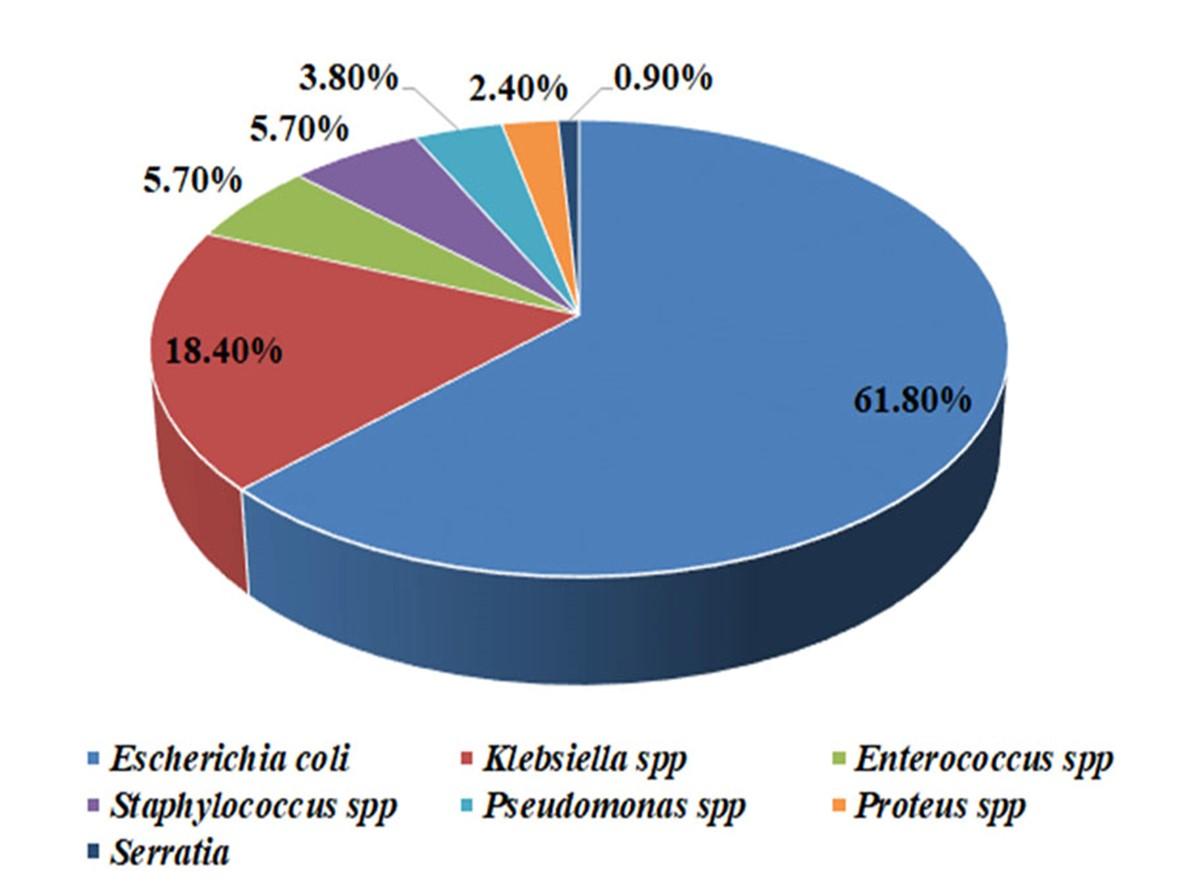
Among 200 samples, results have showed that most causative bacteria are E. coli which is about 61.8% of isolated pathogen as well as 18.4% K. spp, 5.7% E. spp, 5.7% S. spp, 3.8% P. spp, 2.4% P. spp, 0.9% S. spp., and C albicans (0.9%) is also found (Figure 1).
Distribution patterns of gender and age
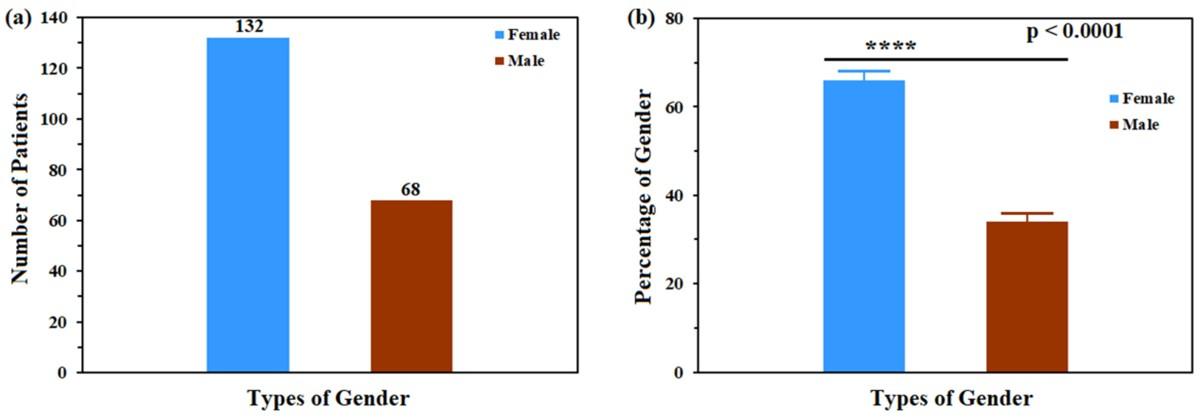
Of the total study population, gender distribution pattern is shown in Figure 2. A total of 1900 urine samples from different ages and sex of suspected UTI patients, 200 urine samples of suspected UTI patients were found as growth positive with UTI. Figure 2 shows the gender distribution pattern, and it represents among the 200 positive patients, 132 female cases and 68 male cases have found with positive UTI with female to male approximate ratio of 2:1. In percentage, it is about 66% female cases and 34% male which is statistically significant with p value ˂0.0001 (Figure 2). Based on the age of the patients, it has also found that older persons are more prevalent for getting UTI which is about 39% with the age group above 55. In case of infant (0-15 years), young people (16-35 years), middle-aged people (36-55 years) are also affected with a percentage of about 10%, 23%, and 28%, respectively shown in Table 1.
Table 1. Frequency and percentage with age range.
Overall antibiotic sensitivity and resistance patterns
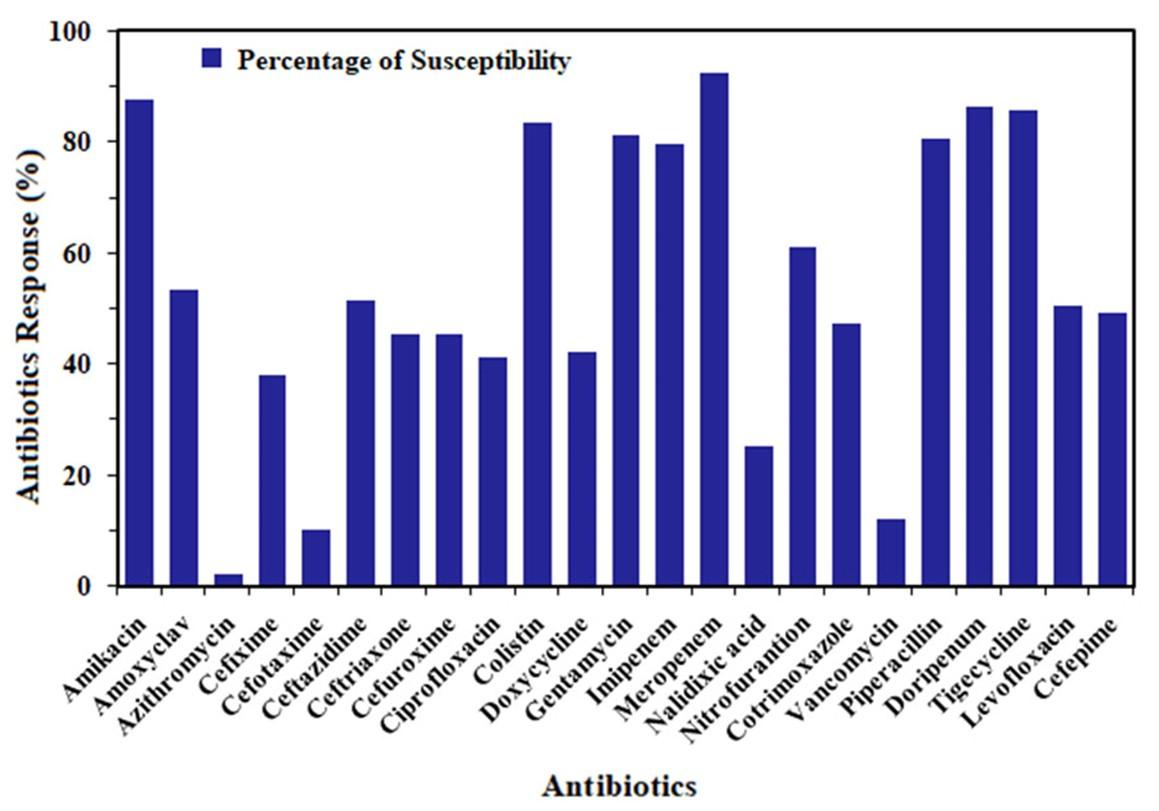
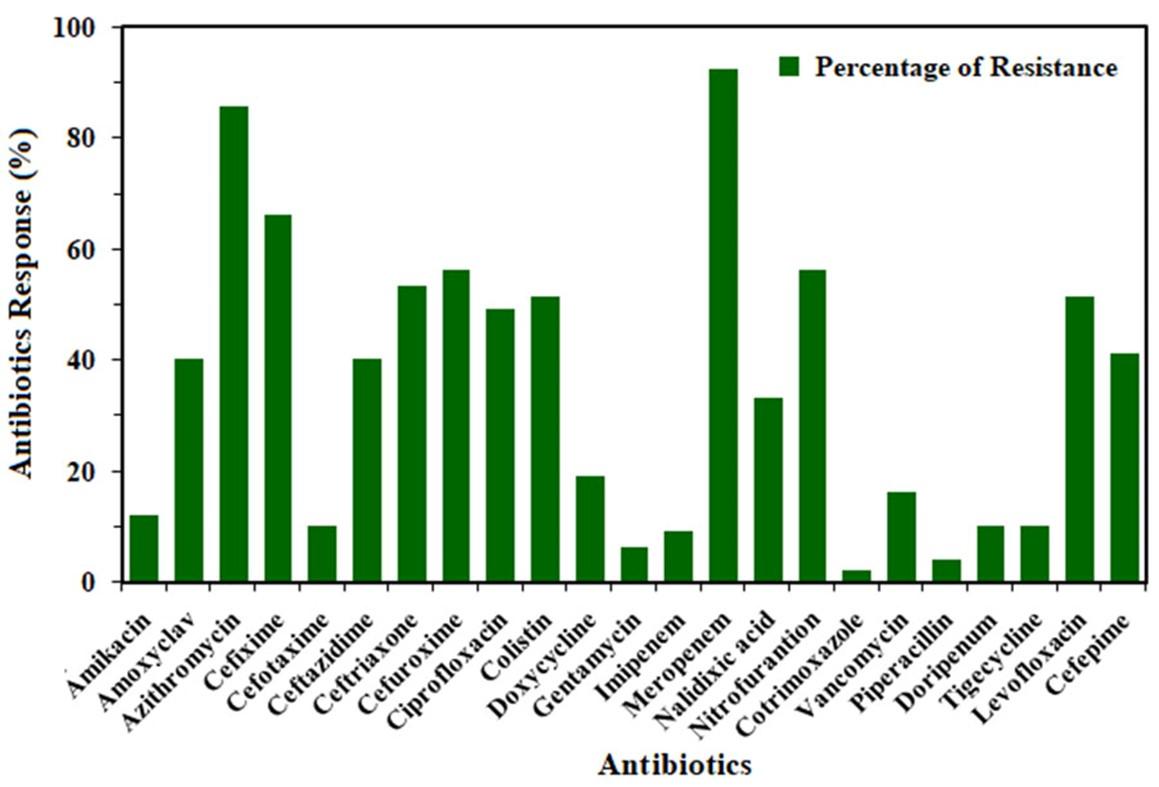
In our study, 23 types of antibiotics were used to show the sensitivity (Table 2) and resistance (Table 3). Highest sensitivity with 91% is shown by antibiotic Meropenem and the lowest sensitivity shown by Cefepime with 48% among the most commonly used antibiotics from 23 types of antibiotics (Figure 3). Azithromycin with 84.4% show the highest percentage of resistance and Ciprofloxacin show the lowest resistance with percentage 46.7% (Figure 4).
Table 2. Percentage of sensitive antibiotics.
Table 3. Percentage of resistant antibiotics.
DISCUSSION
Next to upper respiratory tract infections, UTI is one of the most common infectious diseases, which are often significantly associated with morbidity and mortality. About > 30% of people around world are affected by UTI [22]. The inappropriate administration of antibiotics to treat these infections increased infection resistance to antibiotics [23]. The study attempts to find the most causative bacteria, susceptible hosts, and sensitivity and resistance pattern of antibiotics which are randomly used to treat UTIs. In many perspectives, various researches have been conducted to find out the sensitive antibiotics and tried to suggest the effective drugs. It was determined that E. coli is the most causative bacteria of UTI, followed by K. spp, E. spp, P. spp, P spp, S. spp [24]. As well as percentage of most causative bacterial strains also declared in various research. In our study E. coli showed the highest frequency and percentage; about 61.8% of identified pathogen followed by 18.4 % K. spp, 5.7% E. spp, 5.7% S. spp, 3.8% P. spp, 2.4% P. spp, 0.9% S. While as our findings is quite similar with many other research one is mentioned with percentage: E. coli 59%, K. spp 10%, P. spp 9%, P. spp 15%, E. spp 2.5 % [25].
This study also demonstrates that women are comparatively more likely to UTI than male. In our study 66% female and 34% male (Figure 2) were affected which is highly similar findings with 63% female and 37% male have experienced UTI that are also correlating to previous research. From previous research and our study, it may indicate that women are more likely to develop UTI than men at the age of 35 to 55, patients are more affected. Women get UTIs more often due to shorter urethra (the tube from the bladder to where the urine comes out of the body) of woman's than a man. As women urethral opening is close to both vagina and the anus it makes easier for bacteria to get into the bladder and the main source of germs such as E. coli that cause UTIs [26].
To treat the bacterial infections like UTIs antibiotics are commonly used without checking the antibiotic resistance. However, sometimes antibiotic resistance may occur when bacteria change their response to medicines and develop the ability to beat drugs. Moreover, due to the overuse and misuse of antibiotics has accelerated the process of antibiotic resistance which happened naturally. A growing number of infections are untreatable due to antimicrobial resistance (AMR). The causes of antimicrobial resistance are complex and complicated. They include a lack of adequate health services, badly chosen use of antibiotics both in humans and food animal production, suboptimal water and sanitation systems, gaps in both access and research and development for essential health technologies, and environmental pollution [27]. Some studies show that low-income countries like Bangladesh are more affected by AMR because of the widespread misuse of antibiotics, non-human antibiotic use, poor quality of drugs, inadequate surveillance and factors associated with individual and national poverty indicators like poor healthcare standards, malnutrition, chronic and repeated infections, unaffordability of more effective and costly drugs [28, 29]. Antibiotics such as Meropenem and Amikacin in this study show a good sensitivity profile in the isolates of the urine cultures analyzed, suggesting that they are a good option for the empiric treatment of uncomplicated low UTIs, since they are oral drugs without good Renal penetration. It was also shown that antibiotics such as Azithromycin had a high resistance profile throughout all analyzes. Under this study, 23 types of antibiotics were considered, and the result presents that meropenem, amikacin, gentamycin, piperacillin, imipenem, tigecyclin, doripenum, nitrofurantion were more sensitive antibiotics to UTI among them. This correlates with the study conducted by the research group where Amikacin is the most sensitive antibiotics followed by Imipenem and Meropenem [30]. The percentage of sensitivity was meropenem (91%), amikacin (86.3%), doripenum (84.9%), tegicycline (84.4%), colistin (82.1%), pipercillin (79.2%), imipenem (78.3%), gentamycin (78.3%), nitrofurantion (59.9%) (Figure 3 and Table 2) while as previous study by showed the percentage: nitrofurantion 52%, and cephotaxime 54% [25].
During (2002-2011), fluroquinolone groups were prescribed to treat UTI. Few years later, use of this group of drugs was decreased and use of nitrofurantion was increased as fluroquinolone resistant pathogen developed. Though nitrofurantion is considered as effective antibiotics, it should be avoided by patients of renal disorder [26]. This study mainly focuses on the resistance pattern of antibiotics as well as sensitivity and other factors. It has found that azithromycin, ciprofloxacin, cefuroxime, doxycycline, cefixime, ceftriaxone, cotrimoxazole were resistant antibiotics. The percentage of resistance was azithromycin (84.4%), cefixime (63.2%), cefuroxime (55.2%), ceftriaxone (53.8%), cotrimoxazole (52.4%), doxycycline (48.1%), nalidixic acid (59%) and ciprofloxacin (46.7%) (Figure 4 and Table 3) while a research presented that cotrimoxazole was 91% resistant, amphicillin (87%) and nalidixic acid was 88% resistant [25], ciprofloxacin a fluroquinolone group have already discourage to use for UTI [31]. A study showed that 76.7% E. coli was identified and showed resistance to amphicillin (48.3%), Nalidixic acid (18.6%), Trimethoprim (29.4%). And most effective drugs for susceptible strains was fosfomycin (98.1%), mecillinam (95.8%), aitrofurantion (95.2%) followed by Ciprofloxacin (91.7%), Amoxicillin (82.8%), cefuroxime (82.4%). Klebsiella pneumoniae strains showed resistant to amphicillin, less susceptible to cefuroxime (78.6%), fosfomycin (87.9%), mecillinam (88.8%) [32]. This study has designed to finds out the overall resistance pattern of isolated strains. A study conducted in Dhaka have shown that E. coli is 45% resistant against imipenem, 59% resistant to amikacin, 87% to gentamicin, and 66% to nitrofurantoin [33]. However, in another study, these antibiotics have shown a significant sensitivity to E. coli, which is conducted in Mymensingh city [34]. According to the findings of our study, ciprofloxacin has the lowest resistance percentage, at 46.7%, while azithromycin has the highest resistance percentage, at 84.4%. Globally, antibiotic resistance is rising at an alarming rate. Meropenem and amikacin in this study show a decent responsiveness profile proposing that they are a decent choice for the empiric treatment of simple low UTIs. There is a marked regional variation in the resistance pattern of antimicrobials to E. coli. Antimicrobial agents' resistance has been observed to vary by age, gender, and geographical location. In order to provide an effective antibiotic promptly, accurate information regarding these resistance patterns of the current bacteria is required for the appropriate treatment. All things considered, medical care suppliers ought to know about the opposition examples of various uropathogenic microorganisms. We attempted to investigate the overall patterns of antibiotic resistance against the UTI infection in Tangail City, but this may not reflect the entire Bangladeshi situation. Therefore, in order to ascertain the actual circumstances pertaining to multidrug-resistant uropathogenic bacteria in the general population of Bangladesh, a study that is well-organized is required.
CONCLUSION
The current study demonstrates that women are comparatively more likely to UTI than male where 66% female and 34% male were affected. UTI is mainly caused by E. coli, and it shows the prevalent antibiotic resistance and each antibiotic showed resistance in different range. This study has shown that Azithromycin with 84.4% show the highest percentage of resistance and ciprofloxacin show the lowest resistance with percentage 46.7%. Antibiotic resistance is increasing globally at an alarming rate. Antibiotics such as Meropenem and Amikacin in this study show a good sensitivity profile in the isolates of the urine cultures analyzed, suggesting that they are a good option for the empiric treatment of uncomplicated low UTIs, since they are oral drugs without good Renal penetration. Very common bacterial infections like UTI encourage people to choose antibiotics empirically and easily from community pharmacy, this enhancing the development of antibiotic resistance more rapidly. Multi drug opposition is far and wide among uropathogenic microbes. Because of high protection from regularly utilized anti-microbials, urinary parcel contaminations, particularly brought about by E. coli, are presently truly challenging to exactly treat. Prescription of effective antibiotics requires accurate knowledge of local patterns of antimicrobial resistance. Patients with UTIs in Bangladesh may benefit from the improved treatment options uncovered by our study. Global and domestic policies need to control the antibiotic resistance with appropriate medication, sensitivity test, and proper dosage of antibiotics. Self-awareness is also a conventional way to keep the burden under control. UTI related research looks for the current situation of antibiotic resistance and contribute in the way of controlling antibiotic resistance.
ACKNOWLEDGEMENT
We are grateful for the assistance provided by the collaboration between Mawlana Bhasani Science & Technology University and Medinova Hospital, Tangail, Bangladesh.
AUTHOR CONTRIBUTIONS
FAH, MS, SMA, and EJS were involved in data collection and data analysis. FAH and SMA wrote the Manuscript. NA: supervised the project and do the Project development, manuscript editing. AI, KI, NMH and all other authors read, edit, and approved the manuscript.
CONFLICTS OF INTEREST
There is no conflict of interest among the authors.
References
- [1]Foxman B. Epidemiology of urinary tract infections: incidence, morbidity, and economic costs. Am J Med. 2002; 113(1): 5-13.
- [2]Öztürk R, Murt A. Epidemiology of urological infections: a global burden. World J Urol. 2020; 38(11): 2669-2679.
- [3]Ahmed SS, Shariq A, Alsalloom AA, Babikir IH, Alhomoud BN. Uropathogens and their antimicrobial resistance patterns: Relationship with urinary tract infections. Int J Health Sci. 2019; 13(2): 48-55.
- [4]Stamm WE, Norrby SR. Urinary tract infections: disease panorama and challenges. J Infect Dis. 2001; 183: S1-S4.
- [5]Thompson J, Marijam A, Mitrani-Gold FS, Wright J, Joshi AV. Activity impairment, health-related quality of life, productivity, and self-reported resource use and associated costs of uncomplicated urinary tract infection among women in the United States. Plos One. 2023; 18(2): e0277728.
- [6]Flores-Mireles AL, Walker JN, Caparon M, Hultgren SJ. Urinary tract infections: epidemiology, mechanisms of infection and treatment options. Nat Rev Microbiol. 2015; 13(5): 269-284.
- [7]Sabih A, Leslie SW. Complicated Urinary Tract Infections. StatPearls Publishing LLC, 2022.
- [8]Emiru T, Beyene G, Tsegaye W, Melaku S. Associated risk factors of urinary tract infection among pregnant women at Felege Hiwot Referral Hospital, Bahir Dar, North West Ethiopia. BMC Res Notes. 2013; 6: 292.
- [9]Shaikh N, Hoberman A, Mattoo TK: Urinary tract infections in children: Epidemiology and risk factors. UpToDate. Waltham, MA(Accessed on August 10, 2018) 2019.
- [10]Baer RJ, Nidey N, Bandoli G, Chambers BD, Chambers CD, Feuer S, et al. Risk of Early Birth among Women with a Urinary Tract Infection: A Retrospective Cohort Study. AJP Reports. 2021; 11(1): e5-14.
- [11]Renuart AJ, Goldfarb DM, Mokomane M, Tawanana EO, Narasimhamurthy M, Steenhoff AP, et al. Microbiology of urinary tract infections in Gaborone, Botswana. Plos One. 2013; 8(3): e57776.
- [12]Woodford HJ, George J. Diagnosis and management of urinary infections in older people. Clin Med. 2011; 11(1): 80-83
- [13]Zaman SB, Hussain MA, Nye R, Mehta V, Mamun KT, Hossain N. A Review on Antibiotic Resistance: Alarm Bells are Ringing. Cureus. 2017; 9(6): e1403.
- [14]Chokshi A, Sifri Z, Cennimo D, Horng H. Global contributors to antibiotic resistance. J Glob Infect Dis. 2019; 11(1): 36.
- [15]Rahman M, Sarker SD. Antimicrobial natural products. In: Annual Reports in Medicinal Chemistry. Academic Press, 2020, pp 77-113.
- [16]World Health Organization. Antimicrobial resistance: global report on surveillance. WHO press: Geneva, Switzerland, 2014.
- [17]Valenstein P, Meier F. Urine culture contamination: a College of American Pathologists Q-Probes study of contaminated urine cultures in 906 institutions. Arch Pathol Lab Med. 1998; 122(2): 123- 129.
- [18]Coico R: Gram Staining. Curr Protoc Microbiol. 2006; 00(1):A.3C.1-A.3C.2.
- [19]Mohamad NA, Jusoh NA, Htike ZZ, Win SL. Bacteria identification from microscopic morphology using naive bayes. Int. Jo Comput Sci Engg Inform Tec. 2014; 4(2): 1-9.
- [20]Amirreza T, Sanaz A, Mohamados P. Guidelines for quick application of biochemical tests to identify unknown bacteria. Accounts Biotechnol Res. 2018; 2(2): 065-085.
- [21]Cockerill FR, Wikler M, Bush K, Dudley M, Eliopoulos G, Hardy D, et al. Performance standards for antimicrobial susceptibility testing: twenty-second informational supplement. Clinical and laboratory standards institute: Pennysylvania, USA, 2012.
- [22]Bartoletti R, Cai T, Wagenlehner FM, Naber K, Johansen TEB. Treatment of urinary tract infections and antibiotic stewardship. Eur Urol Suppl. 2016; 15(4): 81-87.
- [23]Mortazavi-Tabatabaei SAR, Ghaderkhani J, Nazari A, Sayehmiri K, Sayehmiri F, Pakzad I. Pattern of Antibacterial Resistance in Urinary Tract Infections: A Systematic Review and Meta-analysis. Int J Prev Med 2019; 10: 169.
- [24]Rossignol L, Maugat S, Blake A, Vaux S, Heym B, Le Strat Y, Kernéis S, et al. Risk factors for resistance in urinary tract infections in women in general practice: A cross-sectional survey. J Infect. 2015; 71(3): 302-311.
- [25]Tambekar D, Dhanorkar D, Gulhane S, Khandelwal V, Dudhane M. Antibacterial susceptibility of some urinary tract pathogens to commonly used antibiotics. Afr J Biotechnol. 2006; 5(17): 1562- 1565.
- [26]Najar M, Saldanha C, Banday K. Approach to urinary tract infections. Indian journal of Nephrol 2009; 19(4): 129.
- [27]Velazquez-Meza ME, Galarde-López M, Carrillo-Quiróz B, Alpuche-Aranda CM: Antimicrobial resistance: One Health approach. Vet World. 2022; 15(3): 743-749.
- [28]Ahmed I, Rabbi MB, Sultana S. Antibiotic resistance in Bangladesh: A systematic review. Int J Infect Dis. 2019; 80: 54-61.
- [29]Shibl A, Memish Z, Osoba A. Antibiotic resistance in developing countries. J Chemotherapy. 2001; 13: 40-44.
- [30]Mohammed MA, Alnour TM, Shakurfo OM, Aburass MM. Prevalence and antimicrobial resistance pattern of bacterial strains isolated from patients with urinary tract infection in Messalata Central Hospital, Libya. Asian Pac J Trop Med. 2016; 9(8): 771-776.
- [31]Kobayashi M, Shapiro DJ, Hersh AL, Sanchez GV, Hicks LA. Outpatient antibiotic prescribing practices for uncomplicated urinary tract infection in women in the United States, 2002–2011. Open Forum Infect. Dis. 2016; 3(3): 159.
- [32]Schito GC, Naber KG, Botto H, Palou J, Mazzei T, Gualco L, Marchese A. The ARESC study: an international survey on the antimicrobial resistance of pathogens involved in uncomplicated urinary tract infections. Intl J Antimicrob Ag. 2009; 34(5): 407-413.
- [33]Sultana R, Sarkar PC, Khan J, Datta S. Prevalence of Multi-drug Resistance Pattern of Escherichia coli in Different Ages and Gender of Urinary Tract Infected Patients. Microbiol Res J Int. 2018; 24(2): 1-10.
- [34]Nobel F, Akter S, Jebin RA, Sarker TC, Mizanur M, Rahman SAZ, et al. Prevalence of multidrug resistance patterns of Escherichia coli from suspected urinary tract infection in Mymensingh city, Bangladesh. J Adv Biotechnol Exp Ther. 2021; 4: 256-264.